BREATHE

Effect of Protocolized Weaning With Early Extubation to Noninvasive Ventilation vs Invasive Ventilation on Time to Liberation From Mechanical Ventilation Among Patients With Respiratory Failure
Perkins JAMA 2018;320(18):1881-1888. doi:10.1001/JAMA.2018.13763
Clinical Question
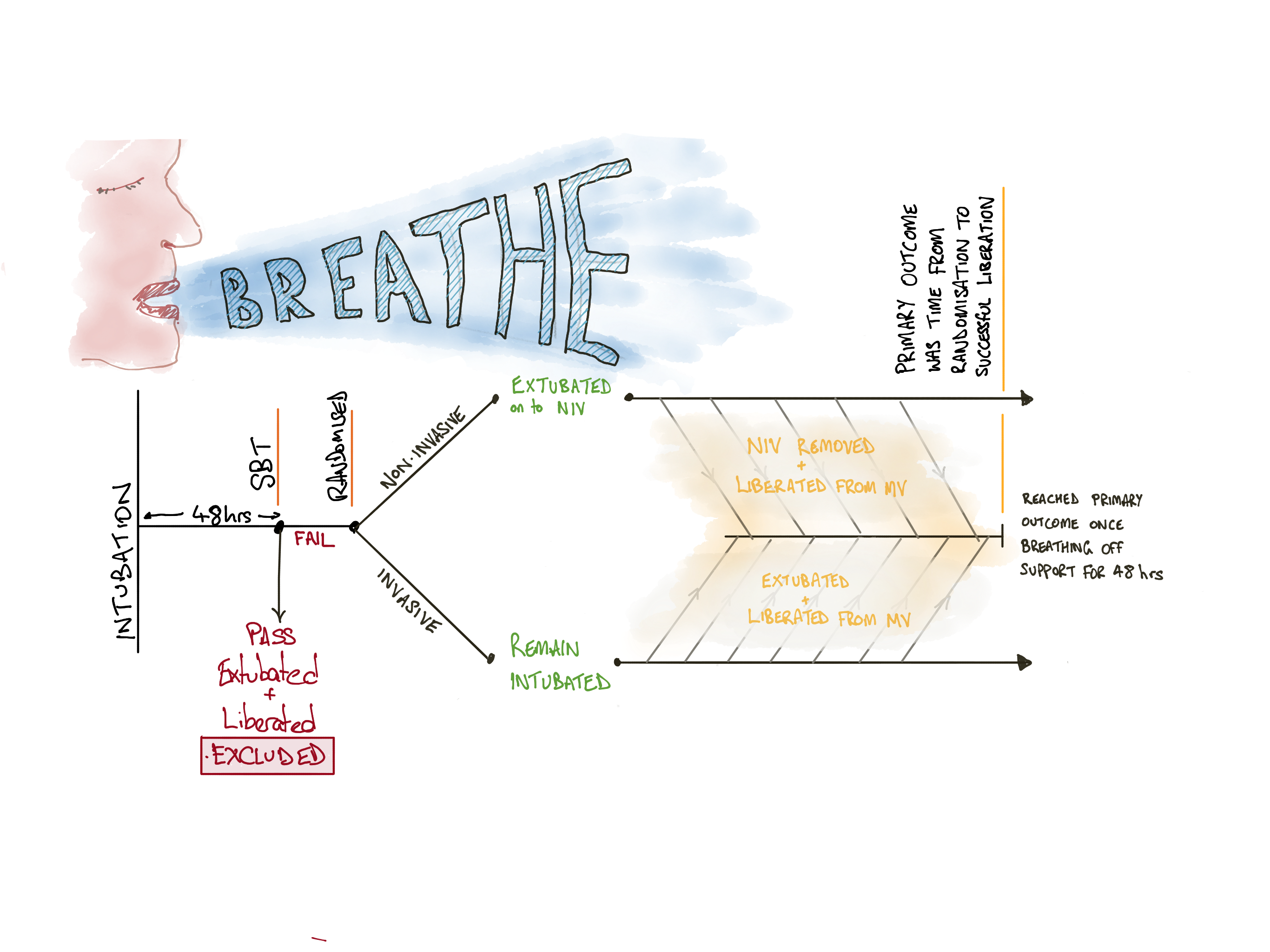
- In adult patients on invasive mechanical ventilation who are difficult to wean, does extubation and weaning on non-invasive ventilation compared to weaning on invasive ventilation reduce the time until liberation from mechanical ventilation?
Background
- Prolonged ventilation is associated with and probably causative of increased morbidity and mortality
- Weaning from mechanical ventilation can be difficult in approximately 1/3 patients, and guidelines recommend breathing trials, optimal (minimal) sedation, protocolised care and early mobilisation, although these are all difficult to implement in complex patients
- Terminology can be confusing, so here are some definitions used within this summary:
- Mechanical ventilation (MV) = positive pressure controlled assisted breathing via either invasive or non-invasive methods
- Weaning = process of transition from mandatory mechanical ventilation to the patient breathing without support, which commences from the time pressure supported ventilation is initiated
- Invasive MV = positive pressure mechanical ventilation applied via an endotracheal tube
- Non-invasive MV = positive pressure mechanical ventilation applied via a face mask (of which there are various designs and sizes)
- Extubation = removal of endotracheal tube from a patient’s airway
- Liberation = cessation of mechanical ventilation so that the patient is spontaneously breathing without pressure support (may still be receiving supplemental oxygen)
Design
- Randomised, controlled trial
- Multi-centre UK-based
- Endorsed by UK Intensive Care Foundation with appropriate ethical approval
- Web-based randomisation method to maintain allocation concealment
- Randomisation in 1:1 ratio with minimisation algorithm
- Stratified by hospital, presence of COPD and post-operative status
- Interventions were not blinded, so all staff were aware of allocation
- Care bundles and criteria for key decision stages were defined to reduce bias from awareness of allocation
- Unrelated therapies and treatments were otherwise at the discretion of the bedside clinician
- Statistical analysis was on principle of intention-to-treat
- Internal pilot study built in to the first 6 months with same trial protocol, and all data included in final analysis
- Initial sample target was 920 but this was drastically reduced after a review of pilot data at the request of the funding body
- This reduction also changed the intended analysis method from the a priori statistical plan that had been published (from competing risks regression model to a Cox proportional hazards model)
- Sample size calculation estimated 364 patients were required for 90% power with the following assumptions
- Median duration of weaning 2.9 days
- Clinically important difference of 1 day
- Defined by clinicians and attention representatives
- Would give a hazard ratio of 1.53
- Statistical significance 0.05
- Sample size inflation by 23% for losses and estimated distribution of outcome (Weilbull distribution with shape parameter = 0.918 and non-constant hazards – this means they expected many early liberations with a few long weaning patients and uncontrolled random factors influencing this)
Setting
- 41 general adult ICUs across United Kingdom
- March 2013 to October 2016
Population
- Inclusion: adult patients on invasive mechanical ventilation through endotracheal tube for more than 48 hours; ready to commence weaning; failed spontaneous breathing trial
- Exclusion: pregnancy; tracheostomy; contraindications to non-invasive ventilation; neurological deficits; home ventilation prior to admission; treatment limitations; need for further surgery or sedation; required equipment not available
- 1752 patients screened; 1388 excluded (95% because they were extubated after a successful breathing trial – that is, they were not difficult to wean from MV); 364 patients randomised
- Baseline characteristics were similar between groups (Invasive weaning vs Non-invasive weaning)
- Mean age: 61.8 vs 64.3 years
- Evidence of delirium: 9.3% vs 12.6%
- Duration of MV prior to randomisation: 4.7 vs 5.3 days
- Admission reason:
- Post-surgical: 21.4% vs 21.4%
- COPD: 3.9% vs 3.9%
- Pneumonia: 40.1% vs 31.3%
- Cardiac: 9.9% vs 14.8%
- Parameters prior to spontaneous breathing trial
- Minute ventilation: 10.5 vs 10.2 l/min
- Resp rate: 21 vs 21
- PEEP: 5 vs 5
- Pressure Support: 11 vs 11 cmH2O
- P:F ratio: 242 (32) vs 227 (30) mmHg (kPa)
- Spontaneous breathing tidal volume: 8.2 vs 7.9 ml/kg
- pH: 7.4 vs 7.4
Intervention
- Non-invasive Ventilation Weaning Protocol
- Patients were extubated and immediately placed on non-invasive mechanical ventilation via a face mask
- Inspiratory positive airway pressure set to pre-extubation pressure support level
- Expiratory positive airway pressure set to pre-extubation positive end-expiratory pressure (PEEP)
- Titrated to achieve patient comfort and less than 30/min respiratory rate
- Reassessed every two hours – if no distress or fatigue:
- Either non-invasive ventilation mask was removed for an unsupported spontaneous breathing trial and liberation from mechanical ventilation
- Or level of positive airway pressure reduced by 2 cmH2O
- Weaning protocol was terminated after 12 hours of unsupported spontaneous breathing
Control
- Invasive Ventilation weaning protocol
- Patients remained intubated and mechanically ventilated via their endotracheal tube
- Reassessed every two hours
- If no distress or fatigue, pressure support was reduced by 2 cmH2O
- If signs of distress or fatigue, reversible causes were treated and / or the pressure support was increased by 2 cmH2O
- Spontaneous breathing trials were performed daily to assess suitability for extubation and liberation from mechanical ventilation
- Weaning protocol was terminated after successful extubation and liberation, or insertion of a tracheostomy
Management common to both groups
- Fraction of inspired oxygen was titrated to maintain SaO2 > 90%
- Active weaning only occurred during daytime hours (8am to 10pm)
- Overnight, unless signs of distress of fatigue developed, patients were rested without ventilator setting changes
- Ventilator care bundles were encouraged, which included head-up position, oral decontamination, sedation holds and peptic ulcer prophylaxis
- Tracheostomy insertion was not recommended until at least after day 7 of mechanical ventilation
- Criteria for re-intubation was provided for guidance
- Cardio-respiratory arrest
- Significant respiratory pause
- Psychomotor agitation
- Excess respiratory secretions
- Bradycardia < 50bpm or tachycardia > 140bpm
- Unresponsive haemodynamic instability
- Surgery or other procedure requiring deep sedation or anaesthesia
- Other treatments were at the bedside clinician’s discretion
Outcome
- Primary outcome: median time from randomisation to successful liberation from mechanical ventilation for more than 48 hours
- Non-invasive group: 4.3 days
- Invasive group: 4.5 days
- Adjusted Hazard Ratio: 1.1 (95% CI 0.89 to 1.40)
- Secondary outcome:
- Duration of invasive ventilation was less in the non-invasive ventilation group, demonstrating effective separation between the two groups
- Total ventilation duration was less in the non-invasive group
- Antibiotic usage for respiratory infections was less in the non-invasive group
- Total antibiotic duration was not different
- Proportion extubated was higher in the non-invasive group
- Re-intubation rate was higher in the non-invasive group but the difference was not statistically significant
- Re-intubation criteria were met more frequently (regardless of whether patients were actually re-intubated) in the non-invasive group but again this difference was not statistically significant
- Tracheostomy insertion was less frequent in the non-invasive group but the difference was not statistically significant
- Mortality at 30, 90 and 180 day was not different
- Adverse events did not occur more frequently in either group
- Quality of life was not different between the two groups
- Process measures demonstrated
- Patients in the non-invasive group were extubated earlier (as per the intervention design)
- Those requiring re-intubation in the non-invasive group were re-intubated earlier than those in the invasive group
- Sedation was administered to those in the non-invasive group for fewer days
- The patients in the non-invasive group spent fewer days in intensive care
- The time to tracheostomy was the same in each group
- The per-protocol, subgroup analyses and sensitivity analyses demonstrated no changes in the statistical significance or conclusions
Authors’ Conclusions
- In patients that failed a spontaneous breathing trial during mechanical ventilation, early extubation to non-invasive ventilation did not reduce the time to complete liberation from mechanical ventilation
Strengths
- Important clinical question given the burden of mechanical ventilation on patients and hospital systems
- Appropriate ethical approval and trial oversight
- Wide, multi-pathology inclusion criteria, which improves generalisation to wider populations
- Multi-centre recruitment, which improves generalisation to wider populations
- Randomised and controlled, which reduces confounding biases
- Appropriate ethics approval
- Total concealment of allocation until recruitment and randomisation, which reduces allocation bias
- Protocolised weaning and standardised extubation / re-intubation criteria to guide clinician decision-making, which reduces maintenance bias given the lack of intervention blinding
- Appropriate statistically adjusted analyses of the primary and secondary outcomes, using rate-based analyses rather than event-based analyses, which improves the power of the statistical conclusions
Weaknesses
- UK based, which may limit the extrapolation to other healthcare models
- Majority of cases recruited from 3 sites, reducing generalisability
- Unblinded therapy, with clinicians, patients and data collectors aware of allocation, which increases the possibility and impact of maintenance, performance and detection biases
- The protocolised, sequential weaning process may have delayed liberation from non-invasive or invasive ventilation in some patients, where clinicians felt they were ready for liberation but the protocol mandated continuation though gradual weaning
- This may reduce the generalisability to non-research, real world setting
- The differences between the non-invasive and the invasive arm may have created a difference in the primary outcome by design due to the protocolised care
- Non-invasive arm were weaned and liberated with two-hourly reviews but the invasive arm underwent only a daily spontaneous breathing trial
The Bottom Line
- This complex randomised, controlled trial failed to demonstrate that early extubation to non-invasive ventilation reduced the total time of mechanical ventilation
- I will continue to extubate early and will use non-invasive mechanical ventilation or high-flow nasal oxygen therapy to support patients, with regular audit of re-intubation rates
- The beneficial secondary outcomes demonstrated in this trial, such as reduced antibiotic use, reduced sedation requirement and reduced time in intensive care warrant further investigation and may be motivators to use non-invasive ventilation more after early extubation
External Links
- [article] Effect of protocolized weaning with early extubation to noninvasive ventilation vs invasive weaning on time to liberation from mechanical ventilation among patients with respiratory failure
- [further reading] Weaning from Mechanical Ventilation from LITFL
- [further reading] Weaning from mechanical ventilation editorial to the article in JAMA
- [further reading] Weaning criteria from Tim Walsh
Metadata
Summary author: Duncan Chambler
Summary date: 1 December 2018
Peer-review editor: Adrian Wong