MACMAN
Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation Among ICU patients
Lascarrou, JB et al. JAMA 2017; 317(5): 483-403. don: 10.1001/jama.2016.20603
Clinical Question
- In intensive care patients requiring orotracheal intubation, does video laryngoscopy (VL) compared to the Macintosh direct laryngoscope (DL) increase the frequency of first pass intubation?
Design
- Non-blinded, multicentre, open-label, 2 parallel group RCT
- Randomisation in blocks of 4, balanced and stratified by centre and experience of intubators (“experts” vs “non-experts”)
- “Experts” – 5 years of ICU experience OR 1 year of ICU and 2 years of anaesthesia experience.
- “Non-expert” – All others
- Randomisation sequence generated by blinded statistician
- Computerised allocation provided full concealment
- Both intention to treat and per protocol analyses performed
- Missing data was considered a failed first pass intubation
- 370 participants planned, assuming first pass success rate of 65% with DL, increased to 80% with VL, type I error of 5%, and type II error of 10%
Setting
- 7 ICUs in France
- May – December 2015
Population
- Inclusion:
- ICU admission and need for orotracheal intubation to facilitate mechanical ventilation
- Exclusion:
- Contraindications to oral intubation, e.g. unstable C-spine
- Insufficient time to include and randomise, e.g. cardiac arrest
- Age <18
- Pregnant or breastfeeding
- Correctional facility inmate
- Under guardianship
- Without health insurance
- Refusal by patient or next of kin
- Previous enrolment in an RCT with intubation as the primary end point
- 489 patients screened, 371 randomised
- 186 randomised to VL, 185 randomised to DL (ITT analysis)
- 183 received VL as intended, 182 received DL as intended (per protocol analysis)
- Baseline statistics similar between groups
Intervention
- McGrath MAC Videolaryngoscope (without stylet)
Control
- Macintosh direct laryngoscope with either a 3 or 4 blade
Standard to both groups:
- All physicians in all centres were trained in the use of all equipment on mannequins before starting the studyI All “non-experts” were supervised by an “expert” during the study
- Preoxygenation with device of the intensivist’s choosing
- Non-rebreathe mask of at least 15L/min for >3 mins
- NIV with 100% oxygen for at least 3 mins
- High flow nasal cannula oxygen at 60L/min with 100% oxygen for at least 3 mins
- IV induction with EITHER etomidate 0.2/0.3mg/kg OR ketamine 1-2mg/kg
- Muscle relaxation with suxamethonium 1mg/kg OR rocuronium 1mg/kg (if sugammadex immediately available)
- Cricoid pressure was at user’s discretion
- If first pass failed, individual was allowed to choose between repeat laryngoscopy or alternative device as per French difficult airway guidelines
Outcome
- Primary outcome: Successful first pass intubation, as defined by capnography over 4 breaths or more – no significant difference
- VL 67.7% vs DL 70.3%, absolute difference -2.5%, P= 0.60
- Predefined Secondary outcomes:
- Proportion of patients with successful intubation at any attempt – no significant difference
- Total time to successful intubation – no significant difference
- Proportion of patients with difficult intubation – no significant difference
- Proportion of patients intubated with alternative techniques – no significant difference
- Duration of mandatory ventilation – no significant difference
- ICU length of stay – no significant difference
- Hospital length of stay – no significant difference
- ICU mortality – no significant difference
- 28 day mortality – no significant difference
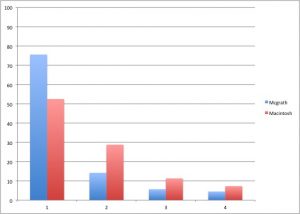
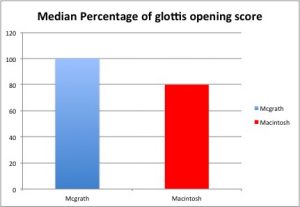
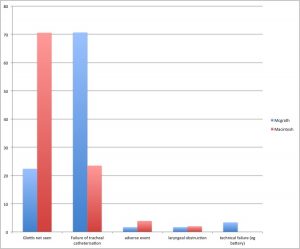
- Cormack and Lehane grade of glottic visibility, % of glottic opening scores, reasons for intubation failure, and severe life threatening complications were significantly different between groups:
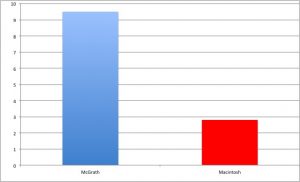
Chart of severe life threatening complications (composite of death, cardiac arrest, severe cardiovascular collapse, and severe hypoxaemia), comparing VL with DL
Authors’ Conclusions
- Amongst patients in ICU requiring intubation, video laryngoscopy compared with direct laryngoscopy did not improve first pass orotracheal intubation rates and was associated with higher rates of severe life-threatening complications
Strengths
- Important clinical question
- Accurate power calculation
- Appropriate methodology with good efforts to minimise bias, such as concealed allocation, maintenance of intended intervention and intention-to-treat analysis
- Objective, patient centred primary outcome
- Registered with clinicaltrials.gov
- All users were familiar with the devices, improving internal validity
Weaknesses
- The intubation protocol allowed for some user variability – this could affect both internal and external validity
- Suxamethonium 1mg/kg was used in the vast majority of intubations – some would debate this would not give optimal conditions for intubation (1.5mg/kg may be better (Naguib et al, 2006)
- Etomidate/sux were used in the vast majority (75-80%) of intubations – this is not common practice worldwide and reduces external validity
- The McGrath is one of many video laryngoscopes
- This trial is really a comparison of the McGrath and the Macintosh, and not a global view of VL versus DL
- In a unit where the McGrath is not the video laryngoscope of choice, I would question the applicability of these results
- The glottic view was significantly improved with the McGrath, however the intubation success was the same – there may have been an issue with technique or training
The Bottom Line
- In this trial comparing the McGrath VL and the Macintosh DL in intubating intensive care patients, there was no difference seen in the primary outcome of first pass success rate
- An association was seen with improved glottic view, and with a worsening of severe complications – however these are secondary outcomes that the study is not powered for and thus hypothesis generating only (and this is clearly stated by the authors in the paper)
- I will focus on gaining expertise with my local devices and protocols, and encouraging my team members to do the same
External Links
- [article] Lascarrou JB et al. Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation among ICU patients. A Randomised clinical trial. JAMA 2017; 317 (5): 483-493 (abstract only)
- [Editorial] O’Gara B et al. Video Laryngoscopy in the Intensive Care Unit. JAMA 2017; 317(5):479-480 (abstract only)
- [Review] Lewis SR et al. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No.: CD011136. DOI: 10.1002/14651858.CD011136.pub2. (free full text)
- [Further reading] Silverberg MJ et al. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation: A randomised control trial. Crit Care Med 2015; 43(3):636-641 (abstract only)
- [Further reading] ICU Revisited. Video Laryngoscopy vs Direct Laryngoscopy. Fooled eyes
Metadata
Summary author: Segun Olusanya
Summary date: 7 April 2017
Peer-review editor: Duncan Chambler




Pingback: The Bottom Line: Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation Among ICU patients – Critical Care Knowledge
Full summary of the MACMAN paper over at JournalBlog.co.uk
This was a well-designed trial with strong internal validity. VL did not improve frequency of first-pass intubation although seemingly contributed to a concerning number of life-threatening complications.
The background of the doctors in the study brings into question its external validity to the UK, where a high proportion of ITU staff have greater anaesthetic experience.
Overall, the trial suggests experience trumps technique.
If my ‘go-to’ device was a videolaryngoscope, and I could always have access to it, I would still use it. If my backup device was a videolaryngoscope, I would still consider it.
Pingback: LITFL Review 277 • LITFL • Life in the Fast Lane Medical Blog
I believe the McGrath blade is a hyperangulated blade. I therefore think the outcome could be attributable to the fact that they didn’t use a stylet during the intubation attempt, which is recommended in a number of guidelines for hyperangulated blades.
This would explain why the views with the VL were superior but lower rates of being able to pass the ETT.