ART
Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators. JAMA. 2017;318(14):1335-1345. doi:10.1001/jama.2017.14171
Clinical Question
- In patients with moderate to severe acute respiratory distress syndrome (ARDS) does use of a lung recruitment maneuver associated with positive end-expiratory pressure (PEEP) titration according to the best respiratory-system compliance, compared with a conventional low-PEEP strategy, decrease 28-day mortality?
Background
- ARDS affects 10-15% of the ICU patient population. ARDS is associated with increased mortality and poor long term quality of life. Mechanical ventilation is a key element of the management of ARDS, yet can also worsen the condition through ventilator-induced lung injury (VILI) and some ARDS patients still progress to ventilator-refractory hypoxaemia.
- An ‘open lung approach’ involving relatively high positive-end expiratory pressure (PEEP) settings and lung recruitment manoeuvres has been proposed as a means of reducing VILI (e.g. by decreasing atelectrauma) and improving oxygenation.
- Recruitment manoeuvres are designed to recruit more alveoli for gas exchange and increase the ventilated lung volume, using brief incremental increases in PEEP. In this study this was followed by down titration of PEEP to the PEEP that achieves the highest level of respiratory-system compliance (ratio of tidal volume to driving pressure), which was then set (+2 cmH2O) as the optimal PEEP
- Previous trials have found improvements in oxygenation, respiratory-system compliance, and biomarkers of systemic inflammation, without increasing barotrauma or other adverse events. However, proof of benefit in terms of patient-orientated outcomes is lacking, despite systematic reviews of pre-existing literature suggesting improved mortality with recruitment manoeuvres and no increase in barotrauma. In general, previous studies have been flawed due to study designs with a high risk of bias and highly variable use of co-interventions in addition to high PEEP and recruitment manoeuvres.
Design
- International Multicenter Randomised Controlled Trial
- Pre-published protocol and statistical analysis plan
- Ethics committees of all institutions approved the study
- Informed consent was obtained from all patients’ representatives
- Eligibility was assessed in two phases:
- The first phase (the screening phase) was the application of inclusion and exclusion criteria (see below)
- The second phase involved patients receiving 3 or more hours of mechanical ventilation following the ARDSNet low-PEEP and low-tidal volume approach
- The FiO2 was then set to 100% and the PEEP to 10 cmH2O for 30 minutes
- PaO2 was then assessed by ABG and the patient was deemed eligible if the PaO2:FiO2 ratio was 200 or lower (and this occurred within 72 hours of the first ratio </= 200 being determined)
- Randomisation
- Randomisation was in a 1:1 ratio using a computer-generated allocation list created by an independent statistician
- conducted with blocks of 4 and stratification by site, age (≤55 years or >55 years) and PaO2:FIO2 ratio (≤100 or >100)
- Allocation concealment via a central web-based system
- Blinding was not possible for the clinicians and outcome assessors, who were aware of the patient’s assigned group following enrolment, however statisticians in charge of analyses were blinded
- Efficacy and safety data were overseen by an independent committee
- Intention-to-treat analysis
- Event-driven study designed to continue until 520 events (28-day deaths) had accrued, which was estimated to provide 90% power, assuming a hazard ratio of 0.75 and type I error of 5%
- Primary outcome was analysed using unadjusted Cox’s proportional hazards models and Kaplan Meier curves
- Data monitoring committee assessed for harm after one-third and two-thirds of the planned sample size were recruited
Setting
- 120 intensive care units from 9 countries (Brazil, Argentina, Colombia, Italy, Poland, Portugal, Malaysia, Spain, and Uruguay)
- November 2011 to April 2017
Population
- Inclusion criteria:
- Patients receiving invasive mechanical ventilation with moderate to severe ARDS of less than 72 hours of duration
- ARDS was defined according to the American-European Consensus Conference criteria, and those with a PF ratio <200 (i.e. moderate severity, or worse) were included
- Exclusion criteria:
- Age younger than 18 years
- Use of vasoconstrictor drugs in increasing doses over the past 2 hours or mean arterial pressure (MAP) less than 65 mm Hg
- Contraindications to hypercapnia, such as intracranial hypertension or acute coronary syndrome
- Pneumothorax, subcutaneous emphysema, pneumomediastinum or pneumatocele (pre-existing or high risk of barotrauma)
- Patients in palliative care only; or
- Previously enrolled patients
- 1013 patients were randomised
- 2077 patients screened
- 863 were ineligible (as they met exclusion criteria)
- Mostly PF ratio >200 after standard ventilation (296 patients), increasing vasoconstrictor doses or MAP <65 mmHg (273 patients), or pre-existing/ high risk of barotrauma (139 patients), or contraindication to hypercapnia (129 patients)
- 201 (18.9%) were eligible but were not enrolled for other reasons (mostly lack of consent or unknown reasons)
- Baseline characteristics
- Two-thirds of the patients had septic shock
- Mean number of nonpulmonary organ failures was > 2
- Most ARDS cases were of pulmonary (62.0%) rather than extrapulmonary origin (38.0%)
- In the intervention and control groups, baseline mean (SD) tidal volume and plateau pressures were 5.8 (1.1) and 5.8 (1.0) mL/Kg of predicted body weight, and 25.8 (4.7) and 26.2 (5.2) cmH2O, respectively
Intervention
- Lung recruitment strategy and PEEP titrated according to the best respiratory-system compliance
- 501 patients randomised – all included in primary analysis
- 480 received initial lung recruitment and titration of PEEP
- 21 did not received the planned intervention, mostly due to hypotension (14)
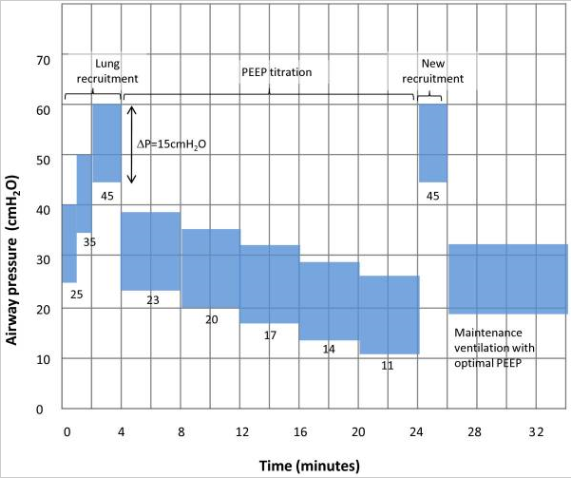
- The patient was put on pressure control ventilation with a driving pressure (difference between plateau pressure and PEEP) of 15 cmH2O
- The patient was initially given a bolus of neuromuscular blocker, then the PEEP was increased to 25 for 1 minute, then 35 for 1 minute, then 45 cmH2O for 2 minutes
- For titration, PEEP was then reduced to 23 cmH2O and the ventilator changed to volume control mode, and PEEP down titrated by 3 cmH2O at a time to a minimum of 11, each step lasting for 4 minutes, after which respiratory-system static compliance was measured
- The optimal PEEP was then taken to be the PEEP at which the highest compliance was achieved, + 2 cmH2O
- After this titration a second round of recruitment was undertaken using a single step of 45 cmH2O PEEP for 2 minutes
- Note that the PEEP values used for recruitment for all patients after the 555th patient were lower and the PEEP down titration was shorter, following a series of cardiac arrests in the intervention group
- Following the recruitment manoeuvre and PEEP titration, tidal volume was maintained between 4–6 ml/Kg predicted body weight to keep plateau pressure ≤ 30 cmH2O
Copied from Trials. 2012; 13: 153. Published online 2012 Aug 28. doi: 10.1186/1745-6215-13-153, and Open Access article distributed under the Creative Commons Attribution License
Control
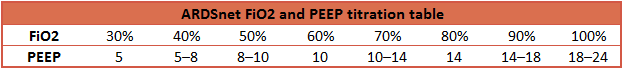
- Conventional ventilation as described by the ARDSnet trial
- No alveolar recruitment manouvres were performed
- PEEP and FiO2 titrated according to ARDSnet published tables
Management common to both groups
- Following the recruitment manouvre and PEEP assignment within the Intervention group, the management of the two groups were the same
- Volume control mode with initial tidal volume 5 ml/kg, titrated within 4–6 ml/kg predicted body weight
- Plateau pressures were limited to ≤ 30 cmH2O
- Ventilatory rate adjusted to be ≤ 35 /min to achieve pH > 7.30
- Management of refractory hypoxaemia was recommended as:
- Prone position
- Nitric oxide
- ECMO
- Pressure support was attempted once PEEP ≤ 14 cmH2O
- Spontaneous breathing trials (SBT) were performed daily with PEEP 5 cmH2O and pressure support 5 cmH2O above PEEP for 30 minutes
- Extubation could be considered if SBT was passed
- Extubation to non-invasive ventilation was recommended
Outcome
- Primary outcome: Mortality at 28 days
- There were 277 deaths (55.3%) in the intervention group (501 patients) and 251 deaths (49.3%) in the control group (509 patients)
- The hazard ratio was 1.20 (95% CI 1.01–1.42; p = 0.041)
- Fragilty Index = 0
- Secondary outcome:
- Death at 6 months was higher at 65.3% in the intervention group (HR 1.18; 95% CI 1.01–1.38; p = 0.04) than the control group (59.9%)
- The intervention group had fewer ventilator-free days between day 1 and day 28 than the control group
- Pneumothorax requiring drainage within 7 days (only cases that were possibly due to barotrauma) was higher among the intervention group (3.2% vs. 1.2%; risk difference 2.0; 95% CI 0.2–3.8; p = 0.03)
- Barotrauma within 7 days (any pneumothorax, pneumo-mediastinum, subcutaneous emphysema, or pneumatocele of more than 2 cm that developed between randomisation and 7 days unless caused by invasive procedure) was also higher among the intervention group (5.6% vs. 1.6%; risk difference 4.0; 95% CI 1.5–6.5; p = 0.001)
- These outcomes were not significantly different:
- Length of stay in ICU
- Length of stay in hospital
- Numerous other exploratory outcomes were used
- Subgroup analyses
- There was no statistically significant difference between subgroups, including:
- PaO2:FiO2 ratio (</= 100 vs >100)
- SAPS 3
- Extra vs Pulmonary ARDS; Duration of ARDS (</= 36 or 37-72 hrs)
- Duration of mechanical ventilation prior to randomisation
- Before vs after the protocol modification
- Per order of enrolment in trial
- There was no statistically significant difference between subgroups, including:
- Lung recruitment
- In 78 cases (15.6%) the recruitment maneuver had to be interrupted, most often due to hypotension or a decrease in oxygen saturation
- The mean (SD) titrated PEEP in the intervention group was 16.8 (3.8) cmH2O
- Lung recruitment was repeated after PEEP titration in 393 patients (78.4%)
- Lung recruitment was not repeated following an initial manoeuvre and PEEP titration from day 1 to 7 in most patients (62.7%)
- 28 patients in the control group received a lung recruitment manoeuvre from days 1-7
- Respiratory/ventilator variables
- The intervention group had higher mean PEEP, higher mean plateau pressure, equivalent tidal volumes and higher PaO2:FiO2 ratios than the control group
- The intervention group did not achieve > 2 cmH2O reduction in driving pressure over days 1-7 compared to the control group
Authors’ Conclusions
- In patients with moderate-to-severe ARDS, a strategy with lung recruitment and titrated PEEP compared with low PEEP increased 28-day all-cause mortality
- These findings do not support the routine use of lung recruitment maneuver and PEEP titration in these patients.
- The authors noted that the intervention group achieved only small increments in respiratory-system compliance and small reductions in driving pressure which may suggest a mild response to the recruitment manoeuvre
- The control group followed a strategy that may have ensured better lung protection than in previous studies, with strictly controlled low tidal volumes and higher PEEP than previous studies
- There may have been some breath stacking which may have contributed to higher driving pressures and barotrauma in the intervention group, though this was not systematically recorded
Strengths
- Multicenter randomised controlled trial with rigorous design, including prepublished protocols and statistical analysis, across 9 countries and 120 ICUs
- Event driven study design ensured adequate events to provide 90% power (assuming HR of 0.75 and type I error of 5%)
- Largest sample size of any lung recruitment trial
- Allocation concealment used
- Intention-to-treat analysis
- Used appropriate statistical tests and sensitivity analyses
- Good baseline balance between the groups
- Minimal loss to follow up – only 3 patients from the control group
- Use of mandated standardised period of ventilation to confirm eligibility prior to enrolment
- Standard volume control mechanical ventilation protocol used across both groups after intervention applied
- Patients in both arms received the interventions as planned
- 95.8% of the intervention group received a lung recruitment manoeuvre
- No evidence that effects changed over time during the 6 year trial, nor that the change to the protocol which occurred around halfway through the recruitment significantly affected the outcome
- Minimal significant difference identified secondary to co-interventions, with only the use of neuromuscular blockers (both events and days used) and the use of sedative infusions (events but not days used) being significantly different between the groups
- Lower overall incidence of barotrauma than in previous studies using high PEEP
Weaknesses
-
- Blinding of patients, treating clinicians, and outcome assessors was not possible due to the nature of the intervention
- May lack external validity to ICUs in other settings due to systemic differences in care delivery (e.g. UK/Europe, North America, Australasia) related to:
- The sites involved (predominantly South American)
- High mortality in both arms, compared to patients of similar ARDS severity in countries such as Australia
- It is unknown if ‘best static pulmonary compliance’ is the optimal means of titrating PEEP (e.g. compared with optimal SpO2 used in the PHARLAP trial)
- High rates of morbidity and mortality temporally associated with recruitment manoeuvres had not been seen in previously published literature
- It is unclear how effect the requirement for “non-escalating noradrenaline” was at excluding under-resuscitated patients who may be more susceptible to haemodynamic compromise from the intervention
- Length of ICU stay and other exploratory outcomes were not included in the original study protocol, but were in the statistical analysis plan
- ARDS is a heterogeneous syndrome, it is still possible that some ARDS subgroups are more likely to benefit, or more likely to be harmed by lung recruitment strategies
- The study did not assess “PEEP responsiveness”, which has been proposed as a potential indicator of patients more likely to benefit from lung recruitment
- The effect of lung recruitment manoeuvres and high PEEP cannot be de-aggregated from one another, or necessary co-interventions such as neuromuscular blockade
- Actual PEEP was a mean of 3 cmH2O higher in the control group than in similar studies using the ARDSNet strategy
- Indeed, anecdotally at least, many clinicians around the world tend to use slightly higher PEEP than prescribed by ARDSNet
- Proning was used as a rescue measure, and was uncommon in both groups (~10% of patients)
- Some ICUs may use proning more liberally than this
- The recruitment and data collection occurred over 6 years, during which time management of ARDS may have changed – although subgroup analysis did not suggest this based on order of enrolment
The Bottom Line
- This trial confirms that protective lung ventilation is the standard of care for moderate-to-severe ARDS and that an open lung approach with recruitment manoeuvres should not be used routinely.
- The increased mortality due to the intervention in this study is statistically fragile and may lack external validity to other settings
- Specific subgroups of ARDS patients may benefit from OLA ventilation with recruitment manoeuvres (e.g. adequately resuscitated patients with PEEP-responsive ARDS and few other risk factors for barotrauma or haemodynamic collapse) but identification of such subroups is uncertain, the evidence for benefit is weak, and there is risk of harm to patients as found in the ART trial
External Links
- [Article] ART trial investigators. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial
- [Further reading] Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials
- [Further reading] Physiologic Responsiveness Should Guide Entry into Randomized Controlled Trials
- [Further reading] Open Lung Approach to Ventilation by LITFL
- [Further reading] Lung Recruitment Manoeuvres
Metadata
Summary author: Emma Browne
Summary date: 5 December 2017
Peer-review editor: Chris Nickson
Additional content: Duncan Chambler



