60/60 sign for Acute PE

Disturbed Right Ventricular Ejection Pattern as a New Doppler Echocardiographic Sign of Acute Pulmonary Embolism
Kurzyna. Am J Cardiology 2002;90:507-511
Clinical Question
- In patients with suspected acute pulmonary embolism, do echo features of disturbed right ventricular ejection allow accurate diagnosis?
Background
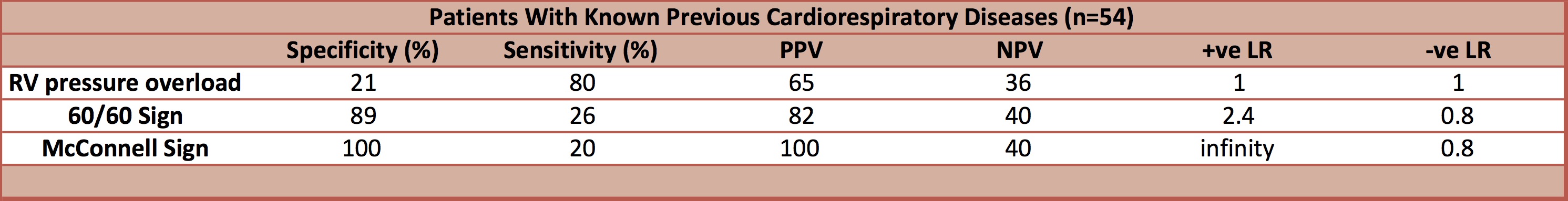
- In patients with acute pulmonary embolism (APE), right ventricular (RV) pressure overload often occurs which can be detected by echocardiography. In patients with pre-existing cardiorespiratory disease the presence of RV overload may be chronic
- A retrospective study suggested that in patients with pre-existing pulmonary hypertension the 60/60 sign may be able to aid in the correct diagnosis of APE
- This study investigated whether the 60/60 sign and McConnell’s sign are useful diagnostic tools in the assessment of suspected APE in patients with and without pre-existing cardiorespiratory disease
Design
- Prospective observational diagnostic cohort
- Consecutive patients
- Not stated if assessors of test of interest were blinded to results of gold standard investigation
- Statistical analysis
- Differences between groups compared with Student’s t test or Mann’s U test
- Differences between categorical variables assessed with Pearson’s chi-square test with Yates’ correction when required
Setting
- Single tertiary pulmonary medicine referral centre, Poland
- Dates of data collection – not documented
Population
- Inclusion criteria: Clinical suspicion of acute pulmonary embolism following clinical assessment including history, examination, arterial blood gases, chest x-ray and ECG
- Exclusion criteria:
- Time from onset or aggravation of symptoms to study enrolment >14 days
- 100 patients included
- 57 male, 43 female
- Age (mean): 61 years ±15 years
- 54 patients had known previous cardiorespiratory disease, including 23 patients with diagnosed/suspected COPD, and 17 patients with congestive heart failure
- 62 patients assessed in the intensive care unit
Tests of Interest
- Trans-thoracic ECHO
- 60/60 sign
- Pulmonary valve acceleration time ≤60ms and tricuspid regurgitation pressure gradient ≤60mmHg
- McConnell sign
- Normokinesia +/or hyperkinesia of the apical segment of the RV free wall despite hypokinesia +/or akinesia of the remaining parts of the RV free wall
- Signs of RV pressure overload, defined as 1 or more of the following signs
- Right sided cardiac thrombus
- RV diastolic dimension on parasternal view of >30mm or a ratio of RV to left ventricle of >1
- Systolic flattening of the interventricular septum
- Pulmonary valve acceleration time <90ms or tricuspid regurgitation pressure gradient >30mmHg in absence of RV hypertrophy
- 60/60 sign
Gold Standard Investigation
- APE diagnosed with
- Spiral CT, n=63 (5mm thick sections, 5mm/s table feed, secondary reconstruction of overlapped images at 3mm intervals)
- High-probability lung perfusion scan, n=1
- Pulmonary angiography, n=1
- Surgery, n=1
- Autopsy, n=1
- APE excluded based on
- Negative CT and negative venous compression ultrasound, n=20
- Negative lung perfusion scan, n=10
- Autopsy, n=3
- Mortality assessed at 1 month
Outcome
- APE confirmed in 67 patients
- 60/60 sign
- Diagnosed 17/67 patients correctly with APE
- 2 false positives (lung fibrosis n=1, ARDS post bi-lobectomy, n=1)
- McConnell Sign
- Diagnosed 13/67 patients correctly with APE
- No false positives
- RV pressure overload
- Diagnosed 54/67 patients correctly with APE
- 18 false positives
- 60/60 sign
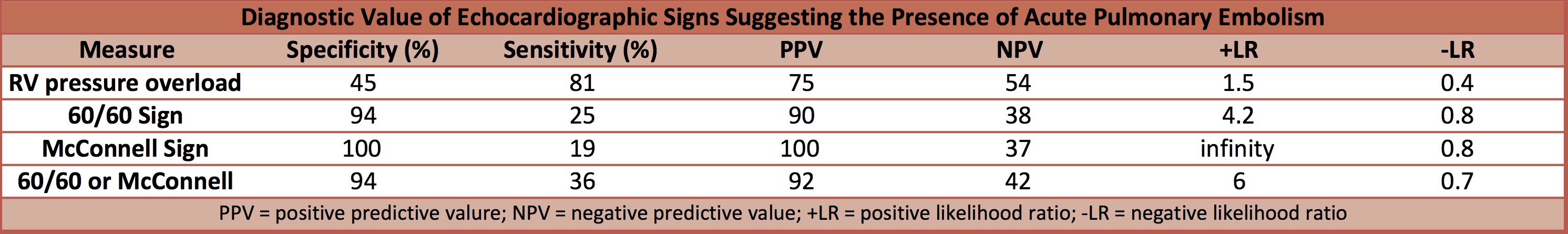
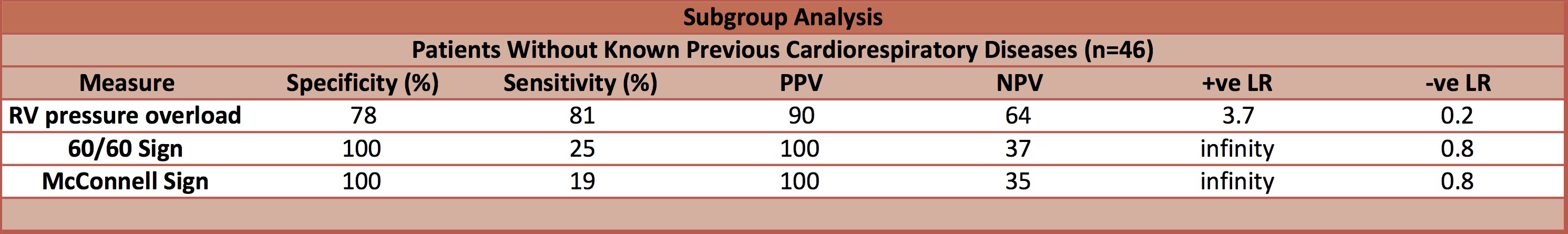
- In patients without known previous cardiorespiratory diseases, the 60/60 sign and McConnell’s sign were 100% specific for the diagnosis of APE
- In patients with APE, comparing patients with a +ve 60/60 sign vs. a –ve 60/60 sign, significant difference in:
- Hypoxaemia: PaO2: 51mmHg vs. 60mmHg, p=0.01
- Collapsibility of inferior vena cava: 19% vs. 33%, p=0.02
- ECHO features in patients with vs. without APE
- RV diameter (mm) measured in parasternal long axis view: 31 vs. 28, p=0.01
- RV:LV ratio: 0.72 vs. 0.63, p=0.04
- Septal flattening: 36% vs. 12%, p=0.02
- Tricuspid regurgitation pressure gradient (mmHg): 41 vs. 28, p=0.01
- Pulmonary valve acceleration time: 73ms vs. 95ms, p<0.0001
- Inferior vena cava expiratory diameter: 18mm vs. 16mm, p=0.06
- IVC collapsibility index: 28% vs. 36%, p=0.22
Authors’ Conclusions
- The 60/60 sign and McConnell signs are reliable but not sensitive signs of APE
Strengths
- Consecutive patients
- Prospective
- Appropriate gold standard
Weaknesses
- Population studied from single tertiary pulmonary referral centre with very high prevalence of APE. This limits the external validity
- Not stated if assessors of test of interest blinded to gold standard investigation
- No sample size calculation
The Bottom Line
- In patients seen at a tertiary referral centre with a high pre-test probability of acute pulmonary embolism, the McConnell Sign had a very high positive likelihood ratio. In patients without previous cardiorespiratory disease the 60/60 sign also demonstrated a very high positive likelihood ratio. A negative McConnell or 60/60 sign added little diagnostic information
- In patients presenting to the ED/ICU with a high probability of acute pulmonary embolism who cannot immediately undergo CT, I will use bedside echo to assess the 60/60 and McConnell’s signs. A positive test result will give me greater confidence for the diagnosis of acute pulmonary embolism, where as a negative result will neither help confirm or repute the diagnosis of acute pulmonary embolism
External Links
- [article] Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism
- [further reading] ECHOPRAXIS – An Echo in PE
- [further reading] Echocardiographic Pattern of Acute Pulmonary Embolism: Analysis of 511 Consecutive Patients
- [further reading] Ultrasound of the week: Pulmonary embolism
Metadata
Summary author: Dave Slessor
Summary date: 10/09/2017
Peer-review editor: Steve Mathieu



