Than
Than: A 2-hour diagnostic protocol for possible cardiac chest pain in the emergency department
Than, JAMA Internal Medicine. 2014,174(1):51-58
Clinical Question
- In patients with suspected acute coronary syndrome does a rapid diagnostic pathway allow early discharge from hospital without more adverse effects when compared with a conventional diagnostic assessment and discharge plan?
Design
- Randomised controlled trial
- Computer generated
- Block Randomisation
- Blinding of personnel determining results of primary outcome
Setting
- Single centre, Emergency Department, New Zealand
- October 2010 – July 2012
Population
- Inclusion: Adult patients with possible cardiac chest pain whose physician planned further observation/troponin testing
- Exclusion: STEMI, other clear cause for chest pain, chest pain >12 hours, persisting chest pain, pregnancy
- 3594 assessed for eligibility of whom 544 randomised
Intervention
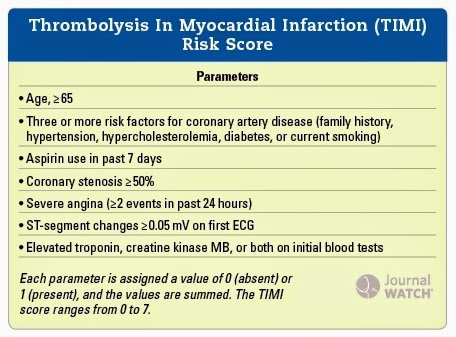
- Low risk patients with a modified TIMI score of 0, and no new ischaemic ECG changes, underwent the rapid diagnostic pathway with a repeat Troponin 2 hours after the initial test.
- If repeat Troponin test normal then patient discharged with outpatient stress test within 72 hours
- If TIMI score >0 or new ischaemic ECG changes, then investigated in standard fashion
(Journal watch – accessed 30th May 2014)
Control
- Repeat Troponin I assay at 6-12 hours
- Follow up investigations at discretion of treating clinician
All Troponin tests were ARCHITECT Troponin I assay in both intervention and control group. This is not a high sensitivity troponin.
Outcome
- Primary outcome: discharge within 6 hours of arrival and without a subsequent major adverse cardiac event (MACE) within 30 days.
- MACE:
- death (unless clearly non-cardiac)
- cardiac arrest
- emergency re-vascularisation
- cardiogenic shock
- ventricular arrhythmia or high degree atrioventricular block requiring intervention
- acute MI
- Significantly more patients were successfully discharged within 6 hours in the intervention group (19.3%) vs. the control group (11%). Difference 8.3% (95% C.I. 1.8-14, P=0.009)
- MACE:
- Secondary outcome: Patients who had a MACE during follow-up (not including initial hospital visit)
- 0.4% in intervention group vs. 0.0% in control group
Authors’ Conclusions
- The rapid diagnostic pathway is an effective and practical strategy to improve early discharge rates for some patients with chest pain
Strengths
- Randomised controlled trial
- Blinding of staff determining primary outcome
Weaknesses
- Not powered to compare rates of MACE between intervention and control groups
- Only 52 patients underwent the rapid diagnostic pathway.
- Patients in the intervention and control group treated differently with regard to the follow up investigations that were arranged.
- All patients that were discharged early had an outpatient stress test within 72 hours. This will limit the external validity of this trial as a number of institutions will not be able to provide this service.
- Single centre
- Only recruited between 0800 – 2200. If people who present at night are different in anyway then this trial may lack external validity.
The Bottom Line
- A rapid diagnostic pathway for patients with suspected cardiac chest pain allowed earlier discharge of some low risk patients. However, further work is necessary before we can tell if this is a safe strategy, and therefore currently this strategy cannot be recommended.
Links
abstract / doi: 10.1001/jamainternmed.2013.11362
Editorial, Commentaries or Blogs
- None
Metadata
Summary author: @DavidSlessor
Summary date: 11 May 2014
Peer-review editor: @stevemathieu75




Pingback: High STEACS – The Bottom Line