Demoule
Neurally adjusted ventilatory assist as an alternative to pressure support ventilation in adults
Demoule A. Intensive care medicine. 2016 Nov 1;42(11):1723-32. doi:10.1007/s00134-016-4447-8
Clinical Question
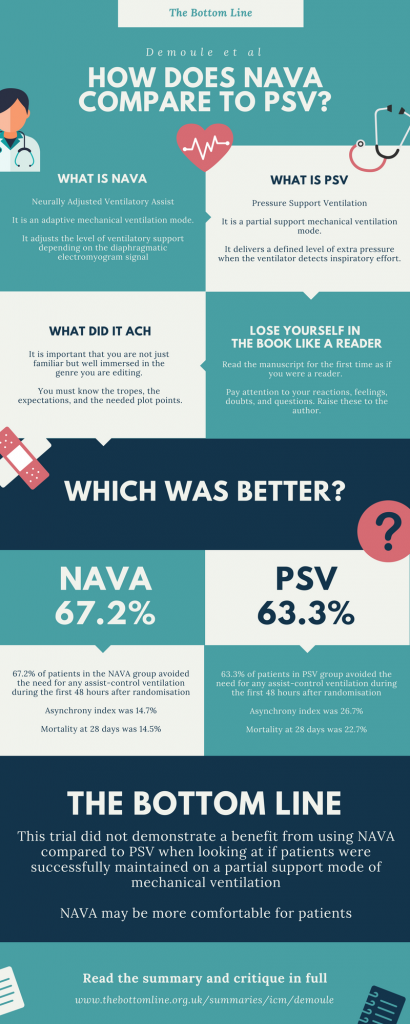
- In intubated patients recovering from acute respiratory failure, does neurally adjusted ventilator assist mode (NAVA) compared to pressure support mode, (PSV) lead to fewer patients returning to assist-control ventilation?
Background
- As patients become more stable, it is common practice to move from assist-control ventilation modes to partial-support ventilation modes
- Assist-control ventilation: VCV by Maquet, S-CMV by Hamilton or IPPV by Drager
- Partial-support ventilation: SIMV, PSV or CPAP-ASB by Drager
- Newer adaptive ventilation modes are becoming available, which may improve patient comfort and reduce the duration of ventilation
- Adaptive-support ventilation: Adaptive Support Ventilation by Hamilton, NAVA by Maquet or Proportional Pressure Support by Drager
- Prior to this trial, NAVA had been tested in small, single centre studies only
Design
- Randomised controlled trial
- Multi-centre
- Block randomisation, stratified by center
- Allocation concealment was achieved by sequentially numbered sealed, opaque, envelopes
- Physicians not blinded but all analyses done blindly
- Intention-to-treat analysis
- Sample size calculation was based on the assumption that 78% of patients will remain in partial ventilator support in the PSV group during the first 48 h
- Allowing for an estimated 10% failure of ventilator data collection, a sample size of 128 patients would provide 80% power at a two-sided alpha level of 0.05 to detect a 17% absolute difference in primary outcome between NAVA group and PSV group
Setting
- 11 ICUs in France comprising 6 medical ICUs, 4 medical-surgical ICUs and 1 surgical ICU
- April 2012 to June 2013
Population
- Inclusion: Patients receiving endotracheal mechanical ventilation for more than 24 h for acute respiratory failure including de novo hypoxaemic respiratory failure, acute cardiogenic pulmonary oedema or acute-on-chronic respiratory failure meeting the following criteria:
- Ability to sustain PSV for at least 30 min with inspiratory pressure below 30 cmH2O
- Estimated remaining duration of mechanical ventilation > 48
- Level of sedation at most 4 on the Ramsay scale in absence of medical decision to increase the level of sedation
- Fraction of inspired oxygen (FiO2) at most 50 % with positive end-expiratory pressure (PEEP) no greater than 8 cmH2O
- Not on high-dose vasopressor therapy defined as norepinephrine above 0.3 μg/kg/min or dopamine above 10 μg/kg/min
- Exclusion:
- Age < 18 years
- Known pregnancy
- Participation in another trial within the 30 days preceding completion of the eligibility criteria
- Contraindication to placement of the NAVA oesophageal tube (i.e. any contraindication to placement of a gastric tube or repositioning of a tube already in place, recent gastrointestinal suture, rupture of oesophageal varices with gastrointestinal bleeding during the 4 days prior to inclusion)
- Decision to withhold life-sustaining treatment
- 3896 screened, 128 randomised, primary outcome available for 118 patients
- Lost to follow-up 7.8%
- Baseline characteristics
- Evenly matched in terms of age, SAPS2 score, duration of mechanical ventilation prior to inclusion and cause of respiratory failure
- Significant baseline differences in terms of gender distribution (more males in NAVA group) and Charlson score (higher degree of comorbidity in PSV group)
Intervention
- NAVA – Neurally Adjusted Ventilatory Assist
- FiO2 and PEEP were defined by treating clinicians according to local guidelines
- NAVA levels were set to obtain a tidal volume of 6-8ml/kg idea body weight
- Continued for 14 days unless patient met criteria for switch to controlled mechanical ventilation or met criteria for weaning and extubation
Control
- PSV – Pressure Support Ventilation
- FiO2 and PEEP were defined by treating clinicians according to local guidelines
- Pressure support levels were set to obtain a tidal volume of 6-8ml/kg idea body weight
Management common to both groups
- EAdi nasogastric catheters were placed in all patients prior to randomisation
- EAdi monitoring data were available to clinicians for patients in both groups
- Criteria for switching to assist-control mechanical ventilation (i.e. failing partial-support ventilation)
- Respiratory distress, hypoxaemia or hypercapnic acidosis despite optimisation of ventilator settings
- Severe hypotension, shock or arrhythmias
- Increased need for sedation for
- Agitation
- Patient–ventilatory asynchrony
- Investigation or procedure
- If criteria for partial-support ventilation were restored, patients remained in the same allocated treatment arm and NAVA or PSV were re-instituted
- Patients were screened for weaning and extubation daily
- If the following criteria were met, a spontaneous breathing trial (up to 1 hour on T-piece or PSV 7 cmH2O with zero PEEP) was conducted and patients were extubated if this was successful
- Improvement in the causative pathology
- SpO2 > 92% on FiO2 < 50% and PEEP < 5 cmH20
- No vasopressor or sedation requirement
- Response to simple commands
- If the following criteria were met, a spontaneous breathing trial (up to 1 hour on T-piece or PSV 7 cmH2O with zero PEEP) was conducted and patients were extubated if this was successful
Outcome
- Primary outcome: Proportion of patients who remained continuously in partial ventilator support mode (either NAVA or PSV) during first 48 hours following inclusion or until extubation without any return to assist-control mode was not different between the groups
- 67.2% (in NAVA group) vs 63.3% (in PSV group)
- Relative risk reduction of 1.19 (95 % CI 0.56–2.54; P = 0.66)
- Absolute risk reduction: 3.91% (95% CI -13.26% to 21.07%, P = 0.70)
- Secondary outcome:
- Patient-Ventilator asynchrony measured by asynchrony index
- 14.7% (12.3-21.7) in NAVA group vs 26.7% (15.8-45.1) in PSV group
- P <0.001
- Dyspnea on day 1 as reported by patients
- 28% in NAVA group vs 66% in PSV group
- P=0.03
- Dyspnea at 48 hours as reported by patients
- 50% in NAVA group vs 52% in PSV group
- P=0.54
- Use of post-extubation non-invasive ventilation
- 43.5% in NAVA group vs 66.6% in PSV group
- P=0.008
- Invasive Ventilator free days at day 7
- 3 (0-4) in NAVA group vs 3 (0-4) in PSV group
- P=0.87
- Invasive Ventilator free days at day 14
- 10 (2.5-11) in NAVA group vs 9 (4.8-11) in PSV group
- P =0.91
- Invasive ventilator free days at day 28
- 24 (10.5-25) in NAVA group vs 23 (13.8-25) in PSV group
- P=0.76
- Death in first 28 days
- 14.5% in NAVA group vs 22.7% in PSV group
- P=0.25
- Days of ICU stay
- 18 (13.5-32) in NAVA group vs 18 (12-26) in PSV group
- P=0.48
- Patient-Ventilator asynchrony measured by asynchrony index
Authors’ Conclusions
- NAVA does not increase the probability of remaining in a partial ventilator mode but decreases patient-ventilator asynchrony and is associated with less frequent application of non-invasive mechanical ventilation post-extubation
Strengths
- Randomised controlled trial
- Multi-centre
- Intention to treat Analysis
- Blinded statistical analysis
Weaknesses
- The primary outcome chosen is not a very patient-important outcome
- Although there was significant difference in use of post-extubation non-invasive ventilation, there were no clearly defined guidelines regarding use of post-extubation NIV
- It was left to the discretion of the physicians who were not blinded
- Although there was significant difference in asynchrony index between the two groups, data for calculating asynchrony index was missing in 14.5% of NAVA group and 24.2% of PSV group
The Bottom Line
- This randomised controlled multi-centre trial failed to demonstrate that NAVA can increase the probability of remaining in a partial ventilator mode in intubated patients recovering from acute respiratory failure
- NAVA was noted to decrease patient-ventilator asynchrony and was associated with less frequent application of non-invasive mechanical ventilation post-extubation
- However, some of the methodical flaws limit the internal validity of the positive findings
- NAVA does not seem to have an advantage over PSV when it comes to patient-significant outcomes such as ventilator free days, length of ICU or hospital stay, mortality etc.
External Links
- [article] Neurally adjusted ventilatory assist as an alternative to pressure support ventilation in adults by Demoule
- [editorial comment] No harm, no benefit: should we give up with neurally adjusted ventilatory assist? by Navalesi
- [corporate product information] NAVA by Maquet
Metadata
Summary author: Vivek Jayaschandran and Alexandra Halalau
Summary date: 21 July 2017
Peer-review editor: Duncan Chambler