ELAIN
Effect of Early vs Delayed Initiation of Renal Replacement Therapy on Mortality in Critically Ill Patients With Acute Kidney Injury
Zarbock. JAMA 2016; 315(20):2190-2199. doi:10.1001/jama.2016.5828
Clinical Question
- In critically unwell patients with acute kidney injury, does early initiation of renal replacement therapy (RRT) compared to delayed initiation reduce all cause mortality at 90 days?
Design
- Randomised, single centre, 2 group, parallel-group trial
- 1:1 randomization between treatment arms
- Block randomization in each stratum with block size of 10
- Group sequential adaptive design with single interim analysis, performed after half the total number of death across both groups
- 230 patients in total required to generate 80% power to detect treatment effect of 18% reduction in 90-day mortality from a baseline of 55% (based on previous literature)
Setting
- University Hospital Munster, Germany
- August 2013 to December 2015
Population
- Inclusion: must have met all five of the following
- Acute kidney Injury- KDIGO stage 2:
- 2-fold increase in serum creatinine from baseline, or urine output <0.5ml/kg/hr for ≥12 hrs despite optimal resuscitation (PCWP>12, CI >2.6, MAP>65, IAP<15)
- NGAL >150ng/dl
- At least one of the following conditions:
- Severe sepsis
- Catecholamines (noradrenaline/adrenaline) >0.1mcg/kg/min
- Refractory fluid overload (worsening pulmonary oedeoma, P/F <300mgHg, fluid balance >10% body weight)
- Development or progression of non-renal organ dysfunction (SOFA organ system score ≥2)
- Age between 18 and 90
- Intention to provide full intensive care treatment for at least 3 days
- Acute kidney Injury- KDIGO stage 2:
- Exclusion:
- Patients with pre-existing kidney disease not requiring RRT
- Patients who had received any previous RRT
- AKI caused by permanent occlusion/surgical lesions of the renal artery
- Obstructive AKI
- HUS/TTP
- Prior Kidney transplant
- Hepatorenal syndrome
- AIDS with CD4 count <0/05 X109/L
- 604 screened, 231 randomised and included in primary analysis
Intervention
- Initiation of RRT within 8 hours of confirmation of KDIGO stage 2
- Delivered to 100% of patients assigned to early group
- Median time to RRT was 6.0 hours (IQR 4.0–7.0)
Control
- Inititation of RRT within 12 hours of either
- KDIGO stage 3 criteria
- Creatinine rise >3 fold increase from baseline, or oliguria <0.3ml/kg/hr for ≥24 hours or serum creatinine > 4mg/dl (353.6 μmol/l) with an acute increase of at least 0.5mg/dl (44.2μmol/l) within 24 hours
- Absolute indication for RRT
- Urea >100mg/dl
- Potassium >6mmol/l and or ECG abnormalities
- Magnesium >4mmol/l and/or anuria/absence of deep tendon reflexes
- Blood pH <7.15
- Urine production <200ml/12hr or anuria
- Organ oedema in the presence of AKI resistant to diuretic treatment (defined as one trial of furosemide)
- KDIGO stage 3 criteria
- Delivered to 91% of patients assigned to delayed group
- Median time to RRT was 25.5 hours (IQR 18.8–40.3)
Common to both groups
- RRT standardized
- CVVHDF
- prediction 100%
- dialysate:replacement fluid ratio 1:1
- effluent flow 30ml/kg
- minimum 110ml/min blood flow
- citrate anticoagulation
- RRT discontinued if renal recovery evident by both:
- > 400ml urine in 24hr without diuretics or > 2100ml in 24hr with diuretics
- creatine clearance > 20ml/min occurred
- RRT could be changed to SLED after 7 days if no recovery
- Additional treatments (ventilation, nutrition) standardized
- Follow up up to 1 year post randomization
Outcome
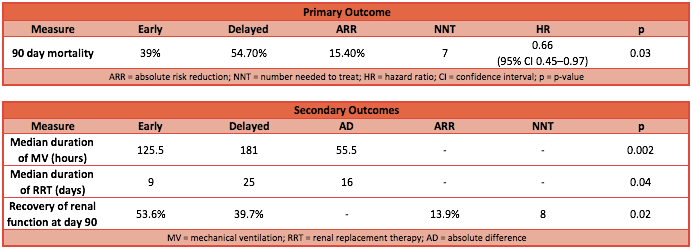
Primary outcome:
- 90 day mortality
- Early group 39.3% vs Delayed group 54.7%
- Hazard ratio 0.66 (95% CI 0.45 to 0.97; P=0.03)
- Absolute risk reduction 15.34% (95% CI 2.62% to 28.06%; P= 0.025)
- Number needed to treat (NNT) is 7
- Fragility Index is 3
- Early group 39.3% vs Delayed group 54.7%
Secondary outcome: early vs delayed
- Median duration of RRT: 9 days vs 25 days (P = 0.04, HR 0.69 [95% CI 0.48–1.00])
- Enhanced recovery of renal function at day 90: 53.6% vs 38.7% (P = 0.02, OR 0.55 [95% CI: 0.32–0.93])
- Median duration of mechanical ventilation: 125.5 hrs vs 181.0 hrs (P = 0.002)
- Error noted in manuscript: should be 181.0 hours not days?
- Length of hospital stay: 51 days vs 82 days (P < 0.001, HR 0.34 [95% CI 0.22–0.52])
- No significant differences seen in
- Requirement of RRT at day 90
- Length of ICU stay
- Adverse events, fluid balance, and RRT modality
- Subgroup analysis of those who reached KDIGO stage 3 vs those who achieved absolute RRT requirement
Exploratory analysis:
- Inflammatory mediators (comparison of MIF, IL-6, IL8, IL-10, IL-18):
- No difference at randomisation
- 24 hours post randomisation: significantly lower IL-6 and IL-8 in early group compared to delayed group (100% of early group and 21.8% of late group had received RRT but this time point)
Authors’ Conclusions
- Amongst critically unwell patients with AKI, early RRT compared with delayed initiation of RRT reduced mortality over the first 90 days
Strengths
- Very strict definitions of AKI used and followed
- No patients lost to follow up, and very little data lost
- Clear separation achieved between groups
- Pre-specified secondary outcome analysis
- Exploratory analysis of inflammatory mediators provides a potential mechanism by which early RRT may improve outcomes
Weaknesses
- Fragility Index 3: a shift of 3 patients would render it non-significant (however, this is greater than the number lost-to-follow-up)
- Single centre study: limits its external validation
- Not all the treatments were standardised between groups. With the groups also being unblinded, this introduces bias, challenging its internal validity.
- External validation further challenged by skewed patient population:
- 216/231 (93.5%) were surgical of which 108 (46.75%) were cardiac surgery patients
- 203 (88%) were mechanically ventilated at time of randomization
The Bottom Line
- This single centre study demonstrates a significant reduction in 90 day mortality with early (stage 2 KDIGO) initiation of RRT, in a group of almost entirely surgical patients. If I worked in this unit or a similar highly surgical ICU, I would consider changing my practice.
- However, other studies challenge these conclusions. A larger multi-centre trial including a more mixed ICU patient population is needed in order to validate these data on a larger scale.
External Links
[article] Effect of Early vs Delayed Initiation of Renal Replacement Therapy on Mortality in Critically Ill Patients With Acute Kidney Injury
[Editorial] Early to Dialyze: Healthy and Wise?
[further reading] Initiation Strategies for Renal Replacement Therapy in the Intensive Care Unit
[further reading] Nephrology journal club: Acute Kidney Injury, when to dialyse.
Metadata
Summary author: Segun Olusanya
Summary date: 15 June 2016
Peer-review editor: Duncan Chambler




Pingback: Editorial: Early vs Late Renal Replacement Therapy – The Bottom Line
Pingback: Keeping Up To Date With The Medical Literature – The Bottom Line
Pingback: ELAIN FOLLOW-UP – The Bottom Line
Pingback: STARRT-AKI – The Bottom Line