NIVAS
Effect of Noninvasive Ventilation on Tracheal Reintubation Among Patients With Hypoxemic Respiratory Failure Following Abdominal Surgery
Jaber. JAMA 2016; 315(13): 1345-1353. doi:10.1001/jama.2016.2706
Clinical Question
- In patients who develop acute hypoxaemic respiratory failure after abdominal surgery, does non-invasive ventilation compared to standard oxygen therapy prevent the need for re-intubation?
Design
- Open-label, randomised, controlled trial
- Design approved and registered in advance: clinicaltrials.gov Id: NCT01971892
- Computer generated randomisation and concealed allocation sequence
- Stratified by study site, age (above or below 60 years), site of surgery (upper vs lower abdomen), use of post-operative epidural analgesia
- Interim blinded reviews at ⅓ and ⅔ recruitment points
- 90% Power to demonstrate superiority of non-invasive ventilation (NIV) against standard oxygen therapy (StdO2) if 300 patients recruited, based upon the following estimates from expert opinion:
- 65% re-intubation rate in StdO2 group
- 40% re-intubation rate in NIV group (i.e. absolute risk reduction of 25%)
- 15% drop out or loss to follow-up
Setting
- 20 Intensive Care Units in France
- May 2013 to September 2014
Population
- Inclusion: Adult patients (>18 years) who had undergone laparoscopic or non-laparoscopic elective or non-elective abdominal surgery under general anaesthesia who develop…
- Acute respiratory failure within 7 days of surgery defined as presence of both
- Hypoxaemia for > 30 minutes (PaO2 < 8 kPa breathing air OR < 10.6 kPa on 15 l/min O2 OR peripheral SpO2 ≤ 90% breathing air)
- Clinical features of respiratory distress (respiratory rate > 30 /min OR intense respiratory muscle work)
- Acute respiratory failure within 7 days of surgery defined as presence of both
- Exclusion: Limits to life-sustaining treatment; contraindications to NIV; sleep apnoea syndrome; need for immediate re-intubation; need for immediate surgical procedure; previous recruitment in research trial
- 535 screened, 300 randomised, 293 included in primary outcome analysis (2.3% loss to follow-up)
- The groups had similar baseline characteristics (NIV vs StdO2):
- Age 64.4 vs 62.5
- BMI 27.1 vs 27.2
- SOFA score 4.5 vs 4.3
- Respiratory rate 28.8 vs 28.2
- Laparoscopic approach 11.1% vs 11.0%
- Epidural analgesia 14.5% vs 15.5%
- Extubated within 6 hours of primary surgery 62.1% vs 63.5%
Intervention
- Non-invasive ventilation (NIV)
- Used from randomisation until day 30 or ICU discharge
- Applied via face-mask using an ICU or NIV-dedicated ventilator with an HME or active humidification
- Inspiratory positive airway pressure (IPAP) started at 5 cmH2O and increased to 15 cmH2O as needed targeting tidal volume (Vt) 6–8 ml/kg predicted body weight
- Positive end-expiratory airway pressure (PEEP, or EPAP) started at 5 cmH2O and increased to 10 cmH2O as needed
- PEEP and inspiratory fraction of oxygen (FiO2) were titrated to maintain SpO2 > 94%
- “Encouraged” to use this for at least 6 hours a day, either continuously or intermittently
- Standard O2 delivered between NIV treatments
- Observed treatment of this group:
- Mean IPAP: 6.7 cmH2O
- Mean PEEP: 5.4 cmH2O
- Mean FiO2: 50%
- Mean Vt: 8.3 ml/kg
- Mean duration of NIV during first day: 7.4 hours
- Proportion given at least 6 hours as intended in first day: 68.9%
- Median total duration of NIV: 4 days
Control
- Standard oxygen therapy (StdO2)
- Supplemental O2 up to 15 l/min to maintain SpO2 > 94%
- Observed treatment of this group:
- 10.4 l/min O2
Management common to both groups
- High-flow oxygen via nasal cannulae were not permitted in either group
- Management and treatment was at the treating clinician’s discretion
- Criteria for re-intubation defined as objectively as possible
- respiratory or cardiac arrest
- respiratory pauses with loss of consciousness or gasping
- massive aspiration
- inability to clear secretions
- heart rate less than 50 ppm with reduced consciousness
- severe haemodynamic instability unresponsive to fluid or vasopressors
- return to theatre (this category was removed for modified intention to treat analysis)
- Invasive ventilation management was a low-tidal volume lung protective strategy
Outcome
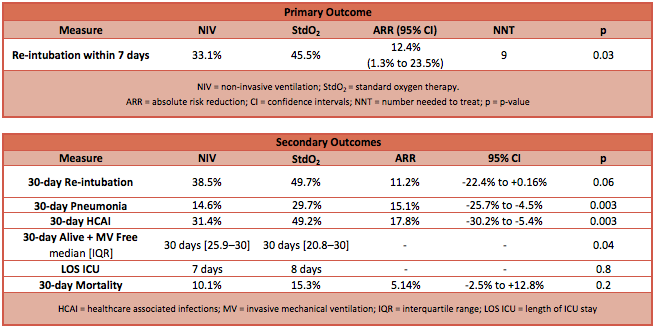
- Primary outcome: The incidence of re-intubation within 7 days of surgery was lower in the NIV group compared to the StdO2 group
- NIV group 33.1% vs StdO2 group 45.5% (ARR 12.4%; 95% CI 1.3% to 23.5%; P=0.03)
- This remained statistically significant in the modified Intention to Treat (mITT) analysis, with the 32 patients re-intubated for surgery removed (representing 11% of patients)
- Number needed to treat (NNT) to prevent one re-intubation: 9 patients
- Fragility Index: 2
- NIV group 33.1% vs StdO2 group 45.5% (ARR 12.4%; 95% CI 1.3% to 23.5%; P=0.03)
- Secondary outcome: see table for data
- Re-intubation rate within 30 days was not different
- Incidence of pneumonia and health-care associated infections was lower in the NIV group
- Days alive and free of invasive mechanical ventilation were greater in the NIV group
- The 30-day mortality ARR point estimate was 5.04%, which gives an NNT of 20 patients, but this was not statistically significant and the 95% confidence intervals of the ARR include -2.5% to 12.8% (slightly harmful to very beneficial)
- There was no difference in the report of adverse events or intolerance to therapy
Authors’ Conclusions
- In patients with established hypoxaemic respiratory failure after abdominal surgery, non-invasive ventilation reduces the risk of re-intubation within 7 days compared to standard oxygen therapy.
Strengths
- Well designed and conducted trial with clear manuscript
- Appropriate methodology for clinical question
- Good internal validity of results however see point about Fragility in weakness section
- Good randomisation and allocation strategy to minimise bias
- Appropriate effort to make outcome objective given it is not possible to blind treating clinicians or patients to allocation
- Small loss-to-follow up relative to primary outcome incidence, and intention-to-treat analysis to minimise bias
- Appropriate statistical methods
- Good external validity (generalisability)
- Multi-centre trial design
- Explicit patient group – high-risk patients having undergone major-complex abdominal surgery
Weaknesses
- Observed rate of re-intubation was lower than expected, so some secondary outcomes that did not demonstrate statistical significance may be Type 2 errors due to the trial being underpowered (this is not relevant to the primary outcome since significance was demonstrated)
- This is particularly relevant to mortality, which would have been a more meaningful outcome to patients and clinicians
- Despite attempts to define an objective primary end-point, bias from unblinded clinicians may have contributed to the significant difference favouring NIV
- The low Fragility Index of 2 highlights how this is not robust evidence – given 7 patients were lost to follow-up and the potential clinician bias in the primary outcome, this is a significant weakness
- Generalising to all health-care systems and patients may not be possible as there was a heavy weighting towards laparotomy (91%) vs laparoscopic (11%) surgery (other surgical factors were reasonably well balanced)
The Bottom Line
- In this trial, 6 hours of low-level non-invasive ventilation in patients with acute hypoxic respiratory failure after major abdominal surgery reduced the need for re-intubation compared to standard oxygen therapy
- Although the significant result is relatively fragile, no clinically relevant harm or intolerance was identified and therefore this paper will change my practice
- Further studies comparing this strategy to high-flow nasal oxygen therapy are urgently needed
External Links
- [article] Effect of Noninvasive Ventilation on Tracheal Reintubation Among Patients With Hypoxemic Respiratory Failure Following Abdominal Surgery
- [further reading] Non-invasive Ventilation by LITFL
- [further reading] Interview with NIVAS first author by ESICM
Metadata
Summary author: Duncan Chambler
Summary date: 18 March 2017
Peer-review editor: Adrian Wong



