POCUS: Moretti
Inferior vena cava distensibility as a predictor of fluid responsiveness in patients with subarachnoid hemorrhage
Moretti. Neurocrit Care. 2010 Aug;13(1):3-9. doi: 10.1007/s12028-010-9356-z
Clinical Question
- In mechanically ventilated patients with subarachnoid hemorrhage (SAH) and a low cardiac index, does the distensibility of IVC on ultrasound, predict fluid responsiveness?
Design
- Prospective observational study
- Consecutive patients
- Statistics:
- No sample size calculation
- Comparisons of:
- Quantitative variables between groups: independent, two-tailed t test
- Categorical data: Fisher’s test
- Repeated measurements: paired t test
- Inter-rater reliability: Pearson’s correlation coefficient
- Blinding: ultrasonographers blinded to haemodynamic parameters and not involved in patient care
- Intra and inter-observer variability of test of interest determined with repeated measurements in 10 patients
Setting
- Single 10 bedded intensive care unit, Italy
- August 2008 and July 2009
Population
- Inclusion criteria:
- Adult patients with SAH (Fisher Grade 3/4)
- Requiring advanced haemodynamic monitoring, sedation, and mechanical ventilation
- Haemodynamic instability: Cardiac index (CI) <2.5 l/min/m2 or a cerebral perfusion pressure (CPP) <60 mmHg
- Exclusion criteria:
- Pre-existing heart failure, cardiac arrhythmias, ARDS, extravascular lung water (ELWI) >14 ml/kg, inability to perform femoral artery cannulation or ultrasonography
- 31 patients recruited. 2 patients excluded, due to suboptimal visualisation of the IVC (n=1), ELWI >14 ml/kg (n=1)
All patients
- Sedated with propofol and remifentanil to achieve bispectral index <60
- Paralysed with cisatracurium. Confirmed with peripheral nerve stimulator
- Given fluid challenge of 7 ml/kg infusion of 6% hydroxyethyl starch over 30 minutes
- Test of interest and gold standard investigation performed at baseline and immediately post fluid challenge
Test of Interest
- IVC sonography
- Performed by 2 intensivists with at least 3 years (60 scans+) ultrasound experience
- Use of 3.5-MHz ultrasound probe
- Performed supine
- During ultrasonography patients ventilated with standardised settings: volume-controlled ventilation, inspiratory:expiratory ratio of 1:2, respiratory rate of 12/min, tidal volume of 8 ml/kg and a positive end-expiratory pressure (PEEP) of 0 cm H2O
- IVC diameter measured in M-mode, 2cm upstream of the origin of the suprahepatic vein. M-mode tracing perpendicular to the IVC
- Maximum IVCD on inspiration (IVCDi) and minimum IVCD on expiration (IVCDe) measured
- IVC distensibility index (dIVC) = (IVCDi-IVCDe)/IVCDe
Gold Standard Investigation
- Thermodilution derived cardiac index
- Measured with femoral PICCO line and internal jugular or subclavian central line
- PEEP set at 5 cm H20 for measurements of stroke volume variation (SVV)
- Patients classified as fluid responsive if cardiac index increased ≥15% with fluid challenge
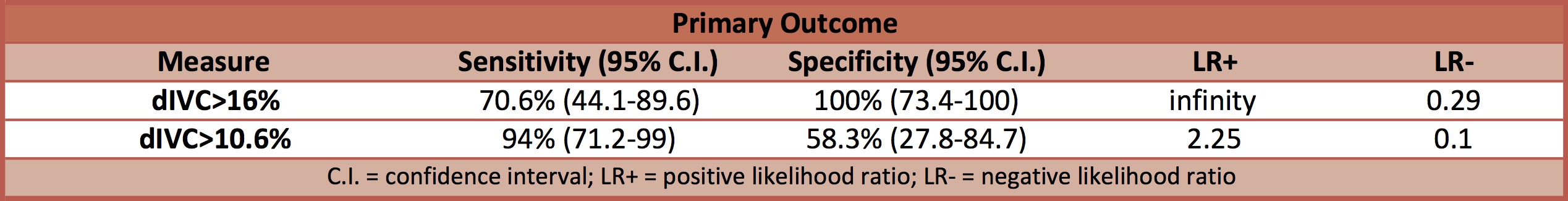
Outcome
- Primary outcome: the reliability of dIVC as a predictor of fluid responsiveness
- Area under the ROC curve
- dIVC: 0.902 (95% C.I. 0.73-0.98)
- Area under the ROC curve
- Secondary outcomes:
- 17 patients classified as fluid responders (FR) and 12 patients classified as non-responders (NR)
- At baseline
- dIVC (%) significantly higher in FR than NR (16 vs. 10, p < 0.0001)
- SVV (%) significantly higher in FR than NR: (11.8 vs. 4.4, p=0.03)
- Post fluid bolus
- In fluid responders significant decrease in
- dIVC (%) 16 ± 3.3 vs. 11.9 ± 2.3, p < 0.001
- SVV (%) 11.8 ± 4.4 vs. 7 ± 2.4, p < 0.001
- In non responders no significant change in
- dIVC (%) 10 ± 3.4 vs. 8.7 ± 2.2, p = 0.42
- SVV (%) 7.5 ± 2.9 vs. 8 ± 4.1, p=0.68
- ROC curves to determine the best predictor of fluid responsiveness: Area under the curve (AUC)
- SVV: 0.779 (95% C.I. 0.587-0.911)
- dIVC: 0.902 (95% C.I. 0.733-0.979)
- CVP: 0.667 (95% C.I. 0.468-0.829)
- In fluid responders significant decrease in
- Intra- and inter-observer variabilities in the measurement of IVCDe were 4 ± 4% and 6 ± 4%, respectively.
Authors’ Conclusions
- IVC distensibility was a reliable measure for predicting fluid responsiveness in critically ill patients with SAH
Strengths
- Blinding of ultrasonographers
- Appropriate gold standard investigation
- Clear description of how test of interest was performed
- Tested for inter and intra-observer variablitiy
Weaknesses
- No sample size calculation, with small numbers of patients included
- External validity may be limited as:
- Restrictive inclusion/exclusion criteria
- PEEP changed to zero for measurement of dIVC. This will not be possible for all patients
- Single centre
The Bottom Line
- In patients with a grade 3/4 SAH and a low cardiac index, who are mechanically ventilated with tidal volumes of 8ml/kg, and are sedated and paralysed, dIVC was a useful predictor of fluid responsiveness. Further trials will need to determine if these results can apply to other populations.
External Links
- [article] Inferior vena cava distensibility as a predictor of fluid responsiveness in patients with subarachnoid hemorrhage
- [further listening] EMCrit – assessing fluid responsiveness
- [further listening] SMACC Debate – Rob MacSweeney vs Paul Marik – Predicting Fluid Responsiveness is a Waste of Time
- [further reading] LITFL fluid responsiveness
- [further listening] EMCrit – IVC Ultrasound for Fluid Tolerance in Spontaneously Breathing Patients
- [further listening] SMACC: The Dark Art of IVC Ultrasound
- [further watching] Ultrasound Podcast: IVC
Metadata
Summary author: David Slessor
Summary date: 25th October 2016
Peer-review editor: Duncan Chambler



