Zochios
The effect of high‐flow nasal oxygen on hospital length of stay in cardiac surgical patients at high risk for respiratory complications
V.Zochios et al. Anaesthesia 2018; 73:1478-1488. doi:10.1111/anae.14345
Clinical Question
- In patients at high risk of respiratory complications after cardiac surgery, does the routine application of high-flow nasal oxygen (HFNO2) compared to standard oxygen reduce hospital length of stay?
Background
- Cardiac surgery patients are at high risk of postoperative pulmonary complications due to a variety of factors. Postoperative pulmonary dysfunction in this population has been termed “inevitable”. High-flow nasal oxygen has gained popularity over recent years and has been investigated in a number of settings, both in theatres and on ICU as a novel method of providing respiratory support for high risk patients.
- Patients with pre-existing respiratory disease are more likely to develop lower respiratory tract infections, have prolonged length of ICU stay and are at increased risk of re-admission to ICU for respiratory support. High-flow nasal oxygen may reduce atelectasis, improve oxygenation and improve clearance of CO2 and respiratory tract secretions hence prevent the development of respiratory failure.
- HFNO2 has been shown to reduce re-intubation rates compared to standard oxygen therapy in both general ICU patients and elective postoperative cardiac surgical patients. It has been found to be non-inferior to BiPAP in patients at high risk of respiratory failure in both general and cardiac ICU settings with regards to re-intubation.
- No previous study has looked at the effect of prophylactic HFNO2 on ICU and hospital length of stay in cardiac surgical patients at high risk of postoperative respiratory complications.
Design
- Single-centre, randomised controlled trial
- Centralised, online 1:1, block randomisation with random block sizes
- Patients and ICU team not blinded but surgical and nursing teams on the surgical ward were unaware of allocation
- Sample size calculation: power of 90% to detect a mean reduction of 2 day in hospital length of stay => 92 patients required
- Increased to 100 to allow for loss to follow up
- Modified intention-to-treat analysis
- Two patients in each group were not extubated by 10am Day 1 postop, 1 withdrew consent and 1 operation was cancelled
Setting
- Single centre trial – Royal Papworth Hospital, Cambridge, UK
- August 2015 – January 2017
Population
- Inclusion:
- Elective cardiac surgery, >18 years old
- ≥1 of the following risk factors:
- formal diagnosis of COPD/Asthma,
- lower respiratory tract infection in preceding 4 weeks, BMI≥35,
- current(within last 6 weeks) heavy smoker(>10 pack years)
- Capable of performing 6-minute walk test (6MWT)
- Exclusion: contraindication to HFNO2 (nasal septal defect), CPAP pre-operatively, patients who did not meet extubation criteria by 10am on first postoperative day
- 1714 patients screened, 100 randomised, 6 excluded from analysis, 94 patients analysed (HFNO2 n=49 vs. Standard oxygen therapy n=45)
- Comparable baseline characteristics including logistic EuroScore
Intervention
- High-flow nasal oxygen therapy (Optiflow® device)
- FiO2 titrated to achieve SpO2≥95%, or ≥93% if at risk of hypercapnoeic respiratory failure. FiO2 actively titrated down to minimum suitable level
- Gas flow: started at 30 L/min, adjusted between 20-50 L/min to achieve respiratory rate <16 and patient comfort
- Could continue on HFNO2 for more than 24h if deemed necessary
Control
- Standard oxygen therapy
- Low flow nasal cannulae or soft facemask
- O2 flow titrated to SpO2≥95%, or ≥93% if at risk of hypercapnic respiratory failure
Management common to both groups
- O2 therapy discontinued after 24h unless evidence of deterioration (desaturation or tachypnoea)
- Standard postoperative respiratory care with regards to physiotherapy, and chest drain removal
- Management of deteriorating patients: increase FiO2, CPAP/Non-invasive Ventilation, and invasive ventilation
Outcome
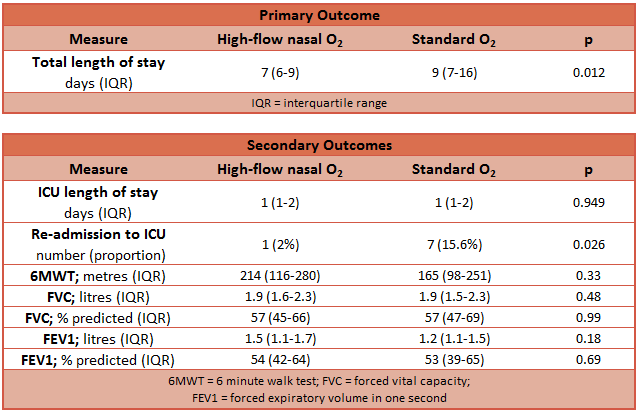
- Primary outcome: Hospital length of stay was less in the HFNO2 group
- Median hospital length of stay
- HFNO2: median 7 days
- Standard O2: median 9 days
- P = 0.012
- Mean hospital length of stay
- Reduced by 29%
- Incidence of prolonged stay (>10 days)
- HFNO2: 18.7%
- Standard O2: 38.6%
- Absolute Risk Reduction: 19.9% (P = 0.026)
- Number needed to treat: 5
- Fragility Index: 1
- Median hospital length of stay
- Secondary outcome:
-
- ICU length of stay: no difference
- ICU re-admission rate: 2% vs. 15.6%, p: 0.026
- NNT: 7.4
- Fragility index: 1
- In-hospital mortality: 1 death in each group
- Extra-pulmonary complications: no difference
- Pulmonary function tests and 6MWT (day 5 or 6 postop)
- Postop pulmonary function tests only performed in two-thirds of patients: no difference
- Postop 6MWT completed by less than half of patients: no difference
- Postoperative quality of recovery (PQRS questionnaire recorded on admission, before discharge and at 1 month postop): no difference in any of the domains
-
Authors’ Conclusions
- The routine use of high-flow nasal oxygen therapy following extubation of cardiac surgical patients with risk factors for postoperative respiratory complications may reduce hospital length of stay and re-admission to ICU
Strengths
- Clearly defined study hypothesis and useful primary outcome
- Appropriate power with prior power calculation for primary outcome
- Well defined inclusion and exclusion criteria
- Appropriate randomisation, with similar baseline Logistic EUROScores
- Surgical and ward nursing staff, who influenced decision to discharge (primary outcome) were unaware of treatment allocation
- Effort to report recovery profiles which is an important patient reported outcome measure
- However unclear how many patients were followed up post-op to provide this data
Weaknesses
- Single centre study, limits generalisability
- Fragility index of 1 for both prolonged length of stay beyond 10 days and ICU re-admission, meaning if a single patient in the control group had a different outcome, the results would lose statistical significance
- Only elective patients who were extubated by the following morning were included in the study and the analysis
- Therefore the results may not be applicable to patients who had emergency surgery or had a longer period of invasive ventilation
- The standard oxygen group had more patients who had a combined procedures
- CABG+valve(s): 8 vs. 13, HFNO2 and standard oxygen respectively
- Combined procedures are associated with higher risk of postoperative complications and prolonged length of stay
- 4 patients in the standard oxygen group crossed over to HFNO2 after 24h, receiving therapy for 48-72 hours
- This may have reduced their risk of re-admission to ICU and improved their recovery, potentially resulting in an underestimation of the intervention effect
- Patients in the HFNO2 group were allowed to remain on this as long as necessary, even after ICU discharge, on the surgical ward
- It is unclear how many patients received HFNO2 therapy, and for how long, beyond the initial 24h period
- If prolonged therapy was common, this may affect generalisability to hospitals where surgical wards don’t provide HFNO2
- Significant attrition at postoperative pulmonary function testing and 6MWT, therefore likely underpowered to show any difference
The Bottom Line
- This was a well-designed and adequately powered RCT with an important and useful primary outcome adding to the growing evidence supporting the use of high-flow nasal oxygen therapy in high risk postoperative patients
- These results are of great importance to all cardiac surgical units and may help inform equipment procurement and staff training to allow increased turnover of patients and reduce the rate of cancellations due to bed shortages
- Based on these results I would strongly consider the use of HFNO2 for postop cardiac surgical patients with additional risk factors for pulmonary complications
- However a larger, multi-centre trial would be desirable to validate the results and improve generalisability
External Links
- [article] The effect of high‐flow nasal oxygen on hospital length of stay in cardiac surgical patients at high risk for respiratory complications: a randomised controlled trial
- [further reading] Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: clinical significance and implications for practice
Metadata
Summary author: Peter Szedlak
Summary date: 23 July 2019
Peer-review editor: Duncan Chambler



