BOX Trial: Blood Pressure

Blood-Pressure Targets in Comatose Survivors of Cardiac Arrest
Kjaergaard et al | New England Journal of Medicine| August 2022
DOI: 10.1056/NEJMoa2208687
Clinical Question
In patients with return of spontaneous circulation (ROSC) after cardiac arrest does a higher MAP target (> 77mmHg) compared to a standard target (>63mmHg) reduce death or survival at discharge with a poor neurological status?
Background
- Manipulation of mean arterial pressure is a central intervention in the ICU to maintain adequate organ perfusion.
- Following cardiac arrest cerebral autoregulation may be impaired and therefore be dependent on adequate perfusion pressure
- Maintenance of higher MAP is likely to require higher doses of vasopressor which may be associated with complications
Design
- Two-centre, double blind, parallel-group randomised clinical trial
- Blinding was achieved by altering the calibration of the invasive blood pressure monitor such that in the intervention group the true blood pressure was 10% higher than the target of 70mmHg and in the control arm the value was 10% lower.
- 2* 2 factorial design (patients also randomised to restrictive or liberal oxygenation – results reported separately)
- Web based randomisation with varying block sizes, stratified by randomisation site
- Further subordinate randomisation to one of two cooling devices for 24 hours (Surface vs Intravascular)
- 800 patients provided between 80 and 90% power to detect a 10% absolute reduction in the primary outcome (a composite of death or discharge from hospital up to ay 90 with a cerebral performance score of 3-4). This was based on a predicted mortality of 38%
Setting
- Conducted in 2 Tertiary Danish ICUs between March 2017 to December 2021
Population
Inclusion Criteria
- Out of hospital cardiac arrest of presumed cardiac cause
- Sustained ROSC > 20mins
- Unconscious (GCS < 9)
Exclusion Criteria
- Females of childbearing potential (unless a negative HCG test can rule out pregnancy within the inclusion window)
- In-hospital cardiac arrest (IHCA)
- OHCA of presumed non-cardiac cause, e.g., after trauma or dissection/rupture of major artery OR cardiac arrest caused by initial hypoxia (i.e., drowning, suffocation, hanging)
- Suspected or confirmed acute intracranial bleeding
- Suspected or confirmed acute stroke
- Unwitnessed asystole
- Known limitations in therapy and Do Not Resuscitate-order
- Known disease making 180 days survival unlikely
- >4hours (240min)from ROSC to screening
- Systolic blood pressure < 80 mmHg despite fluid loading/vasopressor and/or inotropic medication intra-aortic balloon pump/axial flow device
- Temperature on admission<30°C
- 1196 patients assessed for eligibility
- 188 not meeting inclusion criteria.
- Younger than 18 years of age = 9
- OHCA on non-cardiac origin, n=47
- ROSC not sustained > 20 minutes, n=17
- 206 with an exclusion criteria
- 802 randomised
- 403 High target BP group, 9 withdrew consent ITT population of 393
- 399 Low target BP group 3 withdrew consent ITT population of 396
- 188 not meeting inclusion criteria.
Baseline characteristics
High BP target vs Low BP target – very similar between the two groups
- Mean age: 63 vs 62
- Male: 80% vs 81%
- Cardiovascular history
- Hypertension 45% vs 47%
- Diabetes 12% vs 16%
- Myocardial infarction 24% vs 20%
- Atrial Fibrillation 17% vs 15%
- Heart failure 17% vs 18%
- COPD 8% vs 8%
- Stroke 6% vs 9%
- Cardiac Arrest Details
- Shockable rhythm 86% vs 84%
- Witnessed arrest 86% vs 84%
- Bystander CPR 88% vs 87%
- Time to ROSC 21 vs 21 minutes
- Time from arrest to randomisation 150 vs 154 minutes
- Finding and procedures on arrival to hospital
- ST Elevation on ECG 44% vs 47%
- Coronary angiogram performed 93% vs 90%
- pH 7.21 vs 7.22
- Lactate 6.1 vs 5.6
Intervention
-
- Higher MAP target
- Target MAP of 77mmHg for duration of invasive blood pressure monitoring
- Higher MAP target
Control
-
- Standard MAP target
- Target MAP of 63mmHg for duration of invasive blood pressure monitoring.
- Standard MAP target
In both groups
- Protocolised recommendations for achieving MAP with fluids followed by Noradrenaline and then Dopamine.
- Targeted temperature management at 36oC for 24 hours
- Standardised neurological assessment
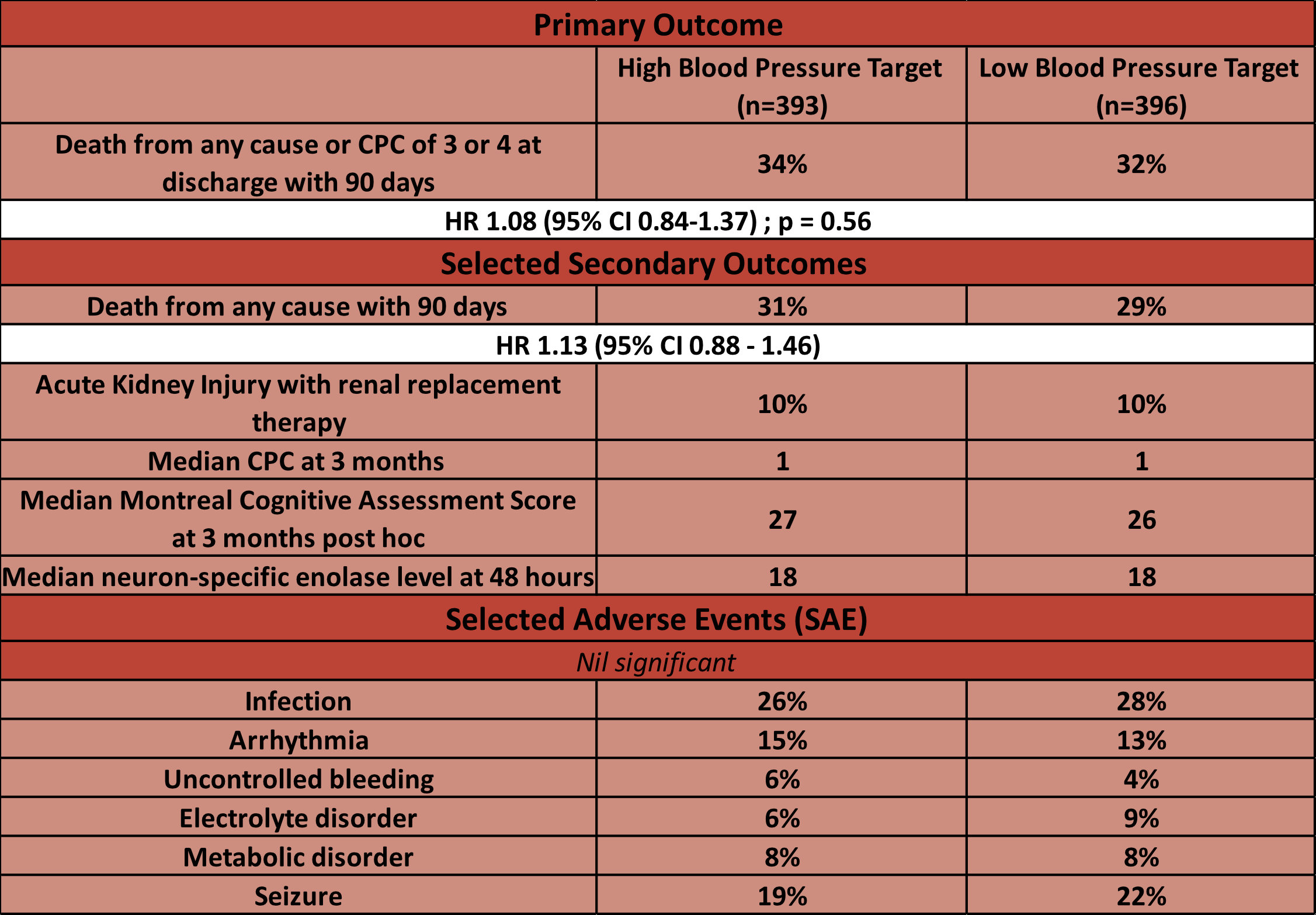
Outcomes
- No significant difference across any outcomes
Sub-groups
- No difference across any pre-specified subgroups for 90 day all-cause mortality
- Age > 64 HR 1.05 (95% CI 0.77-1.44)
- Hypertension HR 1.15 (95% CI 0.81-1.62)
- Renal Impairment HR 0.95 (95% CI 0.39-2.30)
- COPD HR 0.48 (95% CI 0.23-0.99)
- Shockable rhythm HR 1.11 (95% CI 0.85-1.45)
Adverse Events
- Number of moderate and severe bleeding events was not different between groups
- Number of units of packed red blood cells transfused during VA-ECMO was higher in the moderate hypothermia group
- Number of nosocomial infections was not different between groups
Authors’ Conclusions
In comatose survivors of out of hospital cardiac arrest a mean arterial blood pressure of 77 mm Hg as compared with 63 mm Hg did not result in a significant difference in the percent- age of patients who died or had severe disability or coma
Strengths
- Innovative design allowing for double blinding in a haemodynamics trial.
- Good treatment separation between groups (BP 10mmHg and Noradrenaline dose 0.038mcg/kg/min)
- Event rate consistent with predicted reducing risk of type 2 error.
- Well-designed, multi-centre study performed in the emergency setting
- Minimal loss to follow up
- Standardised protocol for temperature regulation
- Similar baseline characteristics between groups
Weaknesses
- Study only performed in two centres in one country which limits generalisability.
- Some may argue that the 10mmHg is not sufficient to difference in outcome
- Large predicted effect size increases risk of type 2 error but no real signal in either direction
- Use of dopamine as inotrope of choice may reduce generalisability
- MOCA scores only available for 359 patients at 3 months making this data harder to interpret
- Did not mandate sedation hold on initial assessment
The Bottom Line
- I will aim to maintain a mean arterial pressure of > 65mmHg for survivors of out of hospital as has been my current practice. It seems any value in this range is likely to be safe
External Links
Metadata
Summary author: Alastair Brown
Summary date: 27th September 2022
Peer-review editor: David Slessor



