AIRWAYS-2
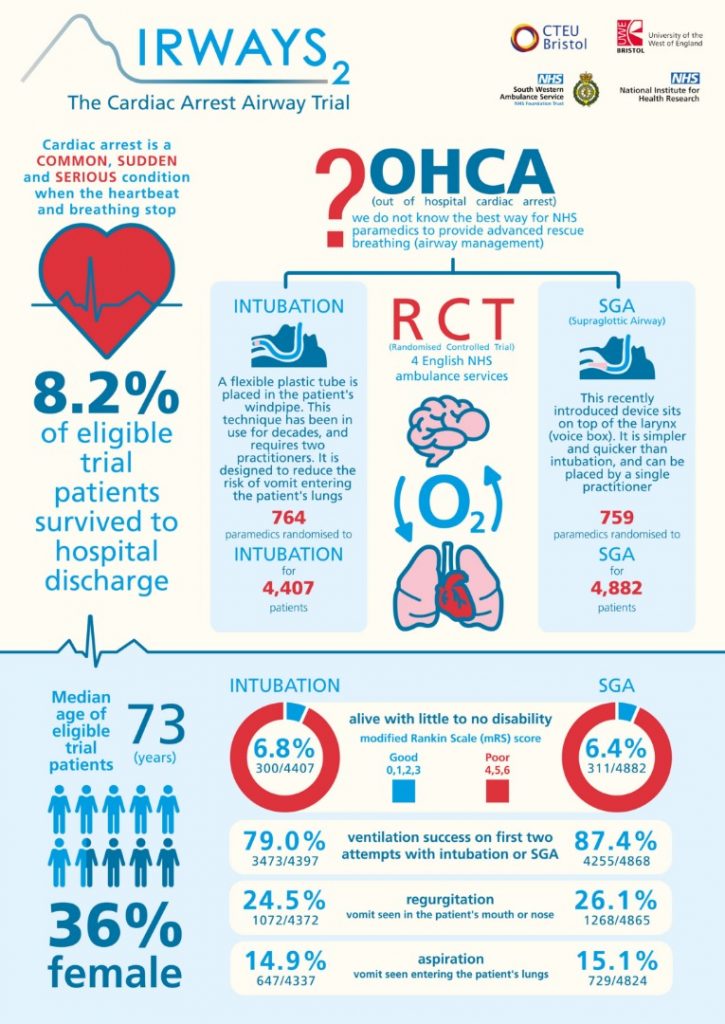
Effect of a Strategy of a Supraglottic Airway Device vs Tracheal Intubation During Out-of-Hospital Cardiac Arrest on Functional Outcome
Benger. JAMA 2018;320(8):779-791. doi:10.1001/jama.2018.11597
Clinical Question
- In adult patients with non-traumatic out-of-hospital cardiac arrest, does a supraglottic airway device compared with tracheal intubation as the initial advanced airway management strategy, improve functional neurological outcome?
Background
- Optimal airway management during out-of-hospital cardiac arrest is uncertain because there is very little high-quality research on which to base treatment recommendations
- The advanced procedure of tracheal intubation has been considered a definitive airway management technique. However, the introduction of a supraglottic airway (SGA) device offers an alternative advanced airway management technique during out-of-hospital cardiac arrest
- Insertion of a SGA device is usually simpler and faster than tracheal intubation and proficiency requires less training and ongoing practice
- Another study (PART) assessing the effect of a strategy of initial laryngeal tube insertion versus endotracheal intubation on 72-Hour Survival in adults with out-of-hospital cardiac arrest was also published in the same issue of JAMA as AIRWAY-2
Design
- Multicenter, cluster randomised trial
- Paramedics from 4 ambulance services in England
- Every eligible patient treated by a participating paramedic was automatically enrolled in the study under a waiver of consent
- Paramedics were randomised in a 1:1 ratio using a purpose- designed secure internet-based system. The computer- generated random sequence was done in advance using varying block sizes and stratified by EMS provider organisation, paramedic experience, and distance from the paramedic’s base ambulance station to the usual destination hospital
- Paramedic discretion with choosing the airway device was permitted and in fact was necessary to secure approval from the research ethics committee and professional support
- 9070 patients in total were needed to detect a difference of 8% vs 10% at the significance level of 5% with 90% power after allowing for clustering. This was based on a previous feasibility study for mortality. There was no data available for the modified Rankin Scale score and an improvement of 2% in the proportion of patients achieving a good outcome (modified Rankin Scale score range, 0-3) was judged to be clinically important
Setting
- 4 ambulance services in England which combined provide service to 21 million people
- June 2015 and August 2017
Population
- Inclusion: Patients aged 18 years or older who had a non-traumatic out-of-hospital cardiac arrest and were treated by a paramedic participating in the trial
- Exclusion: previously recruited to the trial (determined retrospectively); resuscitation deemed inappropriate; advanced airway already in place (inserted by another paramedic, physician, or nurse) when a paramedic participating in the trial arrived at the patient’s side; known to be enrolled in another prehospital RCT; patient’s mouth opened less than 2 cm
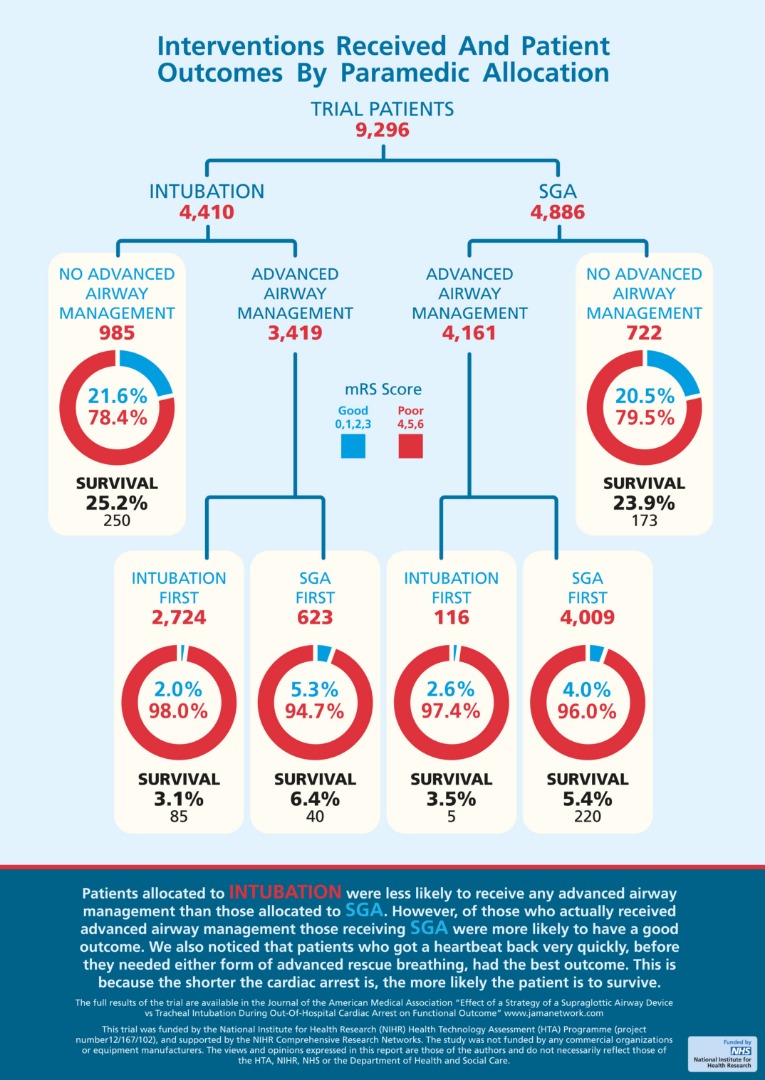
- 9296 patients (4886 in the SGA group; 4410 in the Tracheal Intubation group) were enrolled; 4882 and 4407 patients respectively were included in the primary outcome analysis
- Baseline demographics were well matched:
- median age was 73 years
- 3373 were women (36.3%)
- median time from emergency call to paramedic arrival within one minute between groups
- presenting rhythm (50% asystole; 22% VF)
- witnessed cardiac arrest 63%
- CPR before paramedic arrival 63%
- defibrillation before paramedic arrival 3%
Intervention
- Supraglottic airway device used as initial advanced airway management
- Second generation device with a soft non-inflatable cuff (i-gel; Intersurgical)
- 82% patients received SGA device first
- 15% did not receive airway management
- 2.4% received tracheal intubation first
- Second generation device with a soft non-inflatable cuff (i-gel; Intersurgical)
Control
- Tracheal intubation used as initial advanced airway management
- performed using direct laryngoscopy; video laryngoscopy is not used by paramedics in England
- a 2-person technique using a bougie was recommended
- 62% patients received tracheal intubation first
- 22% did not receive airway management
- 14% received SGA device first
Management common to both groups
- There was a standard approach to airway management (from basic to advanced techniques) which included the use of bag-mask ventilation and simple airway adjuncts prior to advanced airway management
- End-tidal carbon dioxide monitoring was used to confirm correct device placement in all patients.
- All other care was delivered according to standard international resuscitation guidelines
- Paramedics received additional training in their allocated advanced airway management intervention immediately after randomisation. Training comprised theoretical and simulation-based practice over 1 hour with a brief assessment to confirm competence
Outcome
- Primary outcome: There was no statistical difference in the Modified Rankin Scale score at hospital discharge or 30 days after out-of-hospital cardiac arrest, whichever occurred sooner
- In the SGA group, 311 of 4882 patients (6.4%) had a good outcome (modified Rankin Scale score range, 0-3) vs 300 of 4407 patients (6.8%) in the TI group (adjusted risk difference [RD], −0.6% [95% CI, −1.6% to 0.4%])
Modified Rankin Scale score was divided into 2 ranges: 0-3 (good outcome) or 4-6 (poor outcome to death)
- Secondary outcomes, comparing SGA vs intubation
- No significant difference in:
- survival status: died at scene 53.7% vs 56.5%; survived to 30d or hospital discharge 8.0% vs 8.4%
- regurgitation: 26.1% vs 24.5%
- aspiration: 15.1% vs 14.9%
- return of spontaneous circulation at arrival to ED or hospital: 30.6% vs. 28.4%
- Significant difference in:
- Initial ventilation success (<=2 attempts at advanced airway management): 87.4% vs. 79.0%, p<0.001
- Any unintended loss of previously established airway: 10.6% vs. 5.0%, p<0.001
- No significant difference in:
- Sub-group analyses: In patients who received advanced airway management, more patients in the SGA device group had a good outcome
- 163 of 4158 patients (3.9%) vs 88 of 3148 patients (2.6%); adjusted OR, 1.57 [95% CI, 1.18 to 2.07]; risk difference, 1.4% [95% CI, 0.5% to 2.2%])
Reproduced with permission by Airways-2 Trial Investigators and Warwick Print http://www.airways-2.bristol.ac.uk/
Authors’ Conclusions
- Among patients with out-of-hospital cardiac arrest, randomisation to a strategy of advanced airway management with a supraglottic airway device compared with tracheal intubation did not result in a favourable functional outcome at 30 days
Strengths
- A large scale, pre-hospital trial that addresses an important clinical question regarding optimal airway device insertion in a very common presentation
- An important patient focussed primary outcome measure was used
- An excellent summary infographic released with the paper
Weaknesses
- The trial population included patients who did and did not receive advanced airway management
- The use of advanced airway management was greater among paramedics in the SGA device group compared with those in the tracheal intubation group, which could result in confounding by indication
- There was an imbalance in the number of patients in the 2 groups
- There was crossover between the two groups although the authors explain the important of allowing for this on practical and ethical grounds
- The participating paramedics were volunteers, and their airway skills may not be representative of those who chose not to participate in the study
- Although other elements of care (eg, initial basic airway management and subsequent care, such as targeted temperature management and access to angiography) followed established guidelines, between group differences in these factors could have influenced the findings
- The findings may not be applicable in countries with physician-led EMS provision or to another SGA device that may have different characteristics
The Bottom Line
- Among patients with out-of-hospital cardiac arrest, randomisation to a strategy of advanced airway management with a supraglottic airway device compared with tracheal intubation had a comparable functional neurological outcome at 30 days
- Familiarity, competence, and proficiency with the airway device is arguably more important
- Over 1/3 of patients received no bystander CPR and only 322 of 2156 eligible patients (15%) received defibrillation before the paramedics arrived
External Links
- [article] Effect of a Strategy of a Supraglottic Airway Device vs Tracheal Intubation During Out-of-Hospital Cardiac Arrest on Functional Outcome: The AIRWAYS-2 Randomized Clinical Trial
- [further reading] Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial
- [further reading] JC: OOHCA and Airway management. Do we need a tube? St Emlyn’s
- [further reading] EM Nerd-The Case of the Needless Imperative
- [further reading] Emergency Literature of Note: The Great Prehospital Airway Debate
- [podcast] The Resus Room
- [podcast] Phemcast.Podcast: September 2015: The LMA
Metadata
Summary author: Steve Mathieu
Summary date: 6th September 2018
Peer-review editor: Dave Slessor