CULPRIT-SHOCK: One year follow up

One-year outcomes after PCI strategies in cardiogenic shock
Thiele et al. NEJM 2018 DOI: 10.1056/NEJMoa1808788
Clinical Question
- In patients with acute myocardial infarction complicated by cardiogenic shock and evidence of multi-vessel disease on early diagnostic angiography, does immediate multi-vessel percutaneous coronary intervention (PCI) compared to culprit lesion only PCI (with staged revascularisation) improve outcome?
Background
- Early revascularization has been shown to reduce mortality among patients with acute myocardial infarction that is complicated by cardiogenic shock
- Most patients with cardiogenic shock present with multi-vessel coronary artery disease, which is associated with higher mortality than single-vessel disease
- ESC and AHA/ACC 2014 guidelines recommend PCI of all high-grade lesions in patients with acute myocardial infarction complicated by cardiogenic shock, while in haemodynamically stable patients without shock culprit-lesion, only PCI should be preferred
- The 30-day results of the Culprit Lesion Only PCI versus Multi- vessel PCI in Cardiogenic Shock (CULPRIT-SHOCK) trial challenged these guidelines. This study demonstrated the risk of a composite of death from any cause or severe renal failure leading to renal-replacement therapy was lower with culprit-lesion-only PCI
- PCI to culprit lesion is established standard of care but the management of non-culprit lesions is debatable and without longer term follow up
Design
- Prospective, randomised, international multicentre trial
- Open-label
- 1:1 randomisation
- Block randomisation (4 to 6 patients) using internet-based programme
- Stratification according to study centre
- Power calculation
- Baseline 30 day mortality from registries approximately 50% in immediate multi-vessel PCI group and 39% in culprit lesion only PCI group
- 706 patients targeted (assuming 3% dropout) to provide trial with 80% power to detect a difference between the two groups i.e. reject null-hypothesis (alpha 0.048)
Setting
- 83 European centres
- April 2013 – April 2017
Population
- Inclusion:
- Acute myocardial infarction (STEMI or NSTEMI)
- Planned early revascularization by PCI
- Multivessel coronary artery disease defined as >70% stenosis in at least 2 major vessels (≥2 mm diameter) with identifiable culprit lesion
- Systolic blood pressure <90 mmHg for >30 min or catecholamines required to maintain pressure >90 mmHg during systole
- Signs of pulmonary congestion
- Signs of impaired organ perfusion with at least one of the following criteria
- Altered mental status
- Cold, clammy skin and extremities
- Oliguria with urine output <30 ml/h
- Serum lactate >2.0 mmol/l
- Exclusion:
- Resuscitation of >30 minutes
- No intrinsic cardiac activity
- Assumed neurological devastation
- Indication for primary urgent coronary artery bypass grafting (CABG)
- Mechanical cause of cardiogenic shock, or noncardiogenic shock
- Onset of shock >12 hours before randomization
- Age >90 years
- Massive pulmonary embolism
- Known severe chronic kidney disease
- Life expectancy <6 months
- 1075 patients screened, 706 randomised, 686 provided full informed consent
- Total 2 lost to follow up by 1 year
- Median age: 70 years
- Male: 75%
- Number of affected vessels at diagnostic angiography similar in both groups
- 36% with 2 vessel disease
- 63% with 3 vessel disease
Culprit-lesion only PCI
- Culprit-lesion treated first
- All other lesions left untreated at time of initial procedure
- Further staged revascularisation was recommended on the basis of patient’s clinical status and the presence of residual ischaemia on object testing
Multi-vessel PCI
- Culprit-lesion treated first
- All other major coronary arteries with >70% stenosis of diameter (including chronic occlusions) treated
Management common to both groups
- Standard PCI technique with recommended use of drug-eluting stents
- Maximum dose of contrast material = 300 mls
- Transferred to ICU post-intervention for continuous ECG and invasive arterial blood pressure monitoring
- All other therapies (including use of mechanical support devices and renal replacement therapy) left at the discretion of clinical team
- Structured follow up interview at 6 and 12 months
Outcome
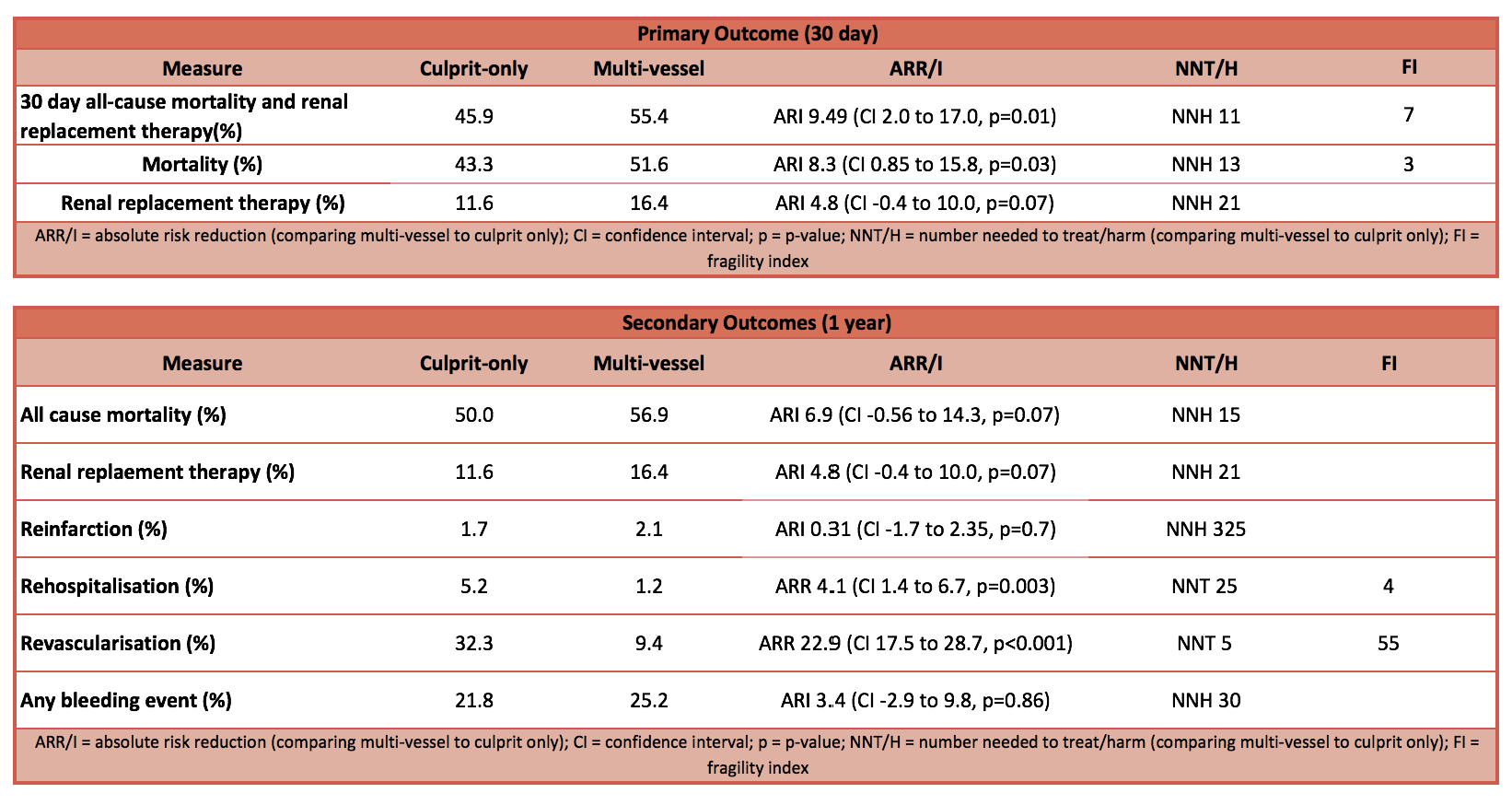
- Primary outcome:
- Composite outcome – 30 day all cause mortality or renal failure leading to replacement therapy favours culprit-lesion only PCI
- Significantly lower in culprit-only PCI (45.9% vs 55.4%; Absolute risk reduction 9.5, CI 2 to 17%, p=0.01, NNT=11)
- Sub-analysis showed that this was primarily due to mortality rather than renal replacement therapy requirements
- Composite outcome – 30 day all cause mortality or renal failure leading to replacement therapy favours culprit-lesion only PCI
- Secondary outcome at 1 year:
- No significant difference between groups
- Death from any cause
- Renal replacement therapy
- Recurrent myocardial infarction
- Bleeding rates
- Culprit-lesion only PCI group had significantly higher
- Staged or urgent repeat revascularisation
- Rehospitalisation for congestive heart failure
- No significant difference between groups
 Authors’ Conclusions
Authors’ Conclusions
- In patients with acute myocardial infarction and cardiogenic shock, 30 days risk of a composite of death from any cause or renal-replacement therapy was significantly lower with culprit-lesion-only PCI than with multi-vessel PCI
- The mortality difference was not significant at 1 year but the incidence of rehospitalisation for heart failure was higher and repeat revascularisation was more frequent with culprit-lesion-only PCI than with multi-vessel PCI
Strengths
- Multi-centre
- Relevant and important clinical question
- Minimal patients lost to follow up
Weaknesses
- The end points in the 1-year analysis are exploratory because the trial was only powered for the 30-day analysis of the primary composite end point
- Open label nature of the study allows for bias in the ascertainment of outcomes and may affect some of secondary outcomes e.g. patients known to be randomised to culprit lesion-only PCI may be more likely to undergo urgent revascularisation due to knowledge that initial revascularisation was targeted
- 43 patients crossed over from culprit-lesion only PCI to multi-vessel PCI (for reasons including lack of haemodynamic improvement, discovery of new lesions after initial PCI), potentially leading to bias toward including more complex and co-morbid patients in the multi-vessel PCI group
- 24% of patients in the multi-vessel arm had a chronic occlusion for which revascularisation was attempted (81% successful). The benefit of revascularisation of chronic total occlusions is unclear particularly in the cardiogenic shock setting, and so mandated revascularisation of these lesions may have contributed to the worse outcomes observed in the multi-vessel PCI group
- 50% of patients required resuscitation prior to PCI, it would be more useful to have neurological status as a more patient-centred outcome
The Bottom Line
- In patients presenting with acute myocardial infarction and cardiogenic shock, a more targeted PCI strategy may be more beneficial excepting that further intervention (PCI and hospitalisation) may be required in the future
- The results of this trial supports the most recent change in European Society of Cardiology Guidelines on Myocardial Revascularisation 2018 where intervention to non-culprit lesions has been downgraded from level II to level III
External Links
- [article] One-year outcomes after PCI strategies in cardiogenic shock
- [article] PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med 2017
- [further reading] 2018 ESC/EACTS Guidelines on myocardial revascularization
- [further reading] ESC 2018 Powerpoint presentation of CULPRIT-SHOCK results
- [further reading] Correspondence to CULPRIT SHOCK
Metadata
Summary author: Adrian Wong
Summary date: 30th August 2018
Peer-review editor: Steve Mathieu



