STITCH (trauma)
 Early Surgery versus Initial Conservative Treatment in Patients with Traumatic Intracerebral Haemorrhage
Early Surgery versus Initial Conservative Treatment in Patients with Traumatic Intracerebral Haemorrhage
Mendelow. Journal of Neurotrauma 2015;32(17):1312-1323. doi:10.1089/neu.2014.3644
Clinical Question
- In patients with traumatic intracerebral haemorrhage (TICH), does early surgery (haematoma evacuation within 12 h of randomisation) compared with initial conservative management reduce major disability and death at 6 months after injury?
Design
- International, multicentre, prospective, patient-randomised, parallel- group pragmatic trial
- Centralised randomisation stratified by geographical region with minimisation procedure based on age group, and severity (measured by pupil equality and reactivity), with a random component (probability of 80%)
- Appropriate concealment of allocation until randomisation
- Open-label – patients, families and treating clinicians aware
- Outcome assessed at 6 months by postal questionnaire or interview assessment (blinded)
- Intention to treat analysis
- Powered at 80% to detect a 10% absolute increase in the rate of favourable outcome from an expected incidence of 50% with conservative treatment and an alpha level of 0.05 if 840 patients were included
- The funding agency decided to halt this study with effect from the end of September 2012 for “failure to recruit in the UK”
- Modified protocol powered at 80% to detect a 21% absolute increase in the rate of favourable outcome from an average favourable outcome of 60%
Setting
- 170 patients randomised from 31 of 59 registered centres in 13 countries worldwide
- December 2009 to September 2012
Population
- Inclusion: TICH patients for whom the treating neurosurgeon was in equipoise about the benefits of early surgical evacuation, compared with initial conservative treatment
- Within 48 h of traumatic brain injury (TBI) and had evidence of a TICH on CT with a confluent volume of greater than 10mL (initially within 24h of TICH but subsequently increased)
- Exclusion:
- significant surface haematoma (extra-dural haemorrhage or subdural haemorrhage) requiring surgery
- 3 or more separate haematomas
- cerebellar haemorrhage/contusion
- where surgery could not be performed within 12 h of randomisation
- severe pre-existing physical or mental co-morbidity
- permanent residence outside a study country
- patient/relative preference for one treatment option
- 1735 patients screened at sites completing logs, (111 were randomised from centres not completing logs)
- Total of 170 randomised, 2 excluded due to different treatment decisions prior to randomisation, 1 lost to follow-up
- 167 analysed in an intention-to-treat analysis (116 received intended treatment)
Intervention
- Early evacuation of the haematoma by a method of the surgeon’s choice (within 12h of randomisation), combined with appropriate best medical treatment
- 21 patients did not receive early surgery as assigned
Control
- Initial conservative treatment was best medical treatment combined with delayed (more than 12 h after randomisation) evacuation if indicated by GCS, neurology and ICP/CPP (cerebral perfusion pressure) in invasively monitored patients
- 31 patients did not receive conservative treatment as assigned
Management Common to Both Groups
- Coagulopathies corrected prior to randomisation
- Best medical treatment could include (depending on the practices within the centre) monitoring of ICP or other modalities and management of metabolism, sodium osmotic pressure, temperature, and blood gasses
- All patients had a CT scan at 5 days (+/–2 days) after randomisation to assess changes in haematoma size
Outcome
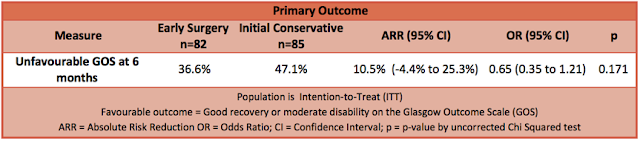
- Primary outcome: A non-significant benefit of early surgery on the dichotomised GOS favourable vs unfavourable outcome
- Favourable = good recovery or moderately dependent
- Unfavourable = severely dependent, vegetative, or dead
- Unfavourable outcome in early surgery group 37% vs initial conservative management group 47% (OR, 0.65; 95% CI 0.35–1.21; p = 0.17)
- Absolute difference of 10.5% (95% CI – 4.4–25.3)
- Sensitivity analysis using logistic regression adjusting for age, volume, and GCS gives an OR of 0.58 (95% CI 0.29–1.16; p = 0.122)
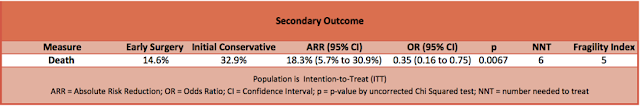
- Secondary outcome: Significant benefit of early surgery on 6-month mortality
- 6-month mortality in early surgery group 15% vs initial conservative patients 33% (OR, 0.35; 95% CI 0.16–0.75; p = 0.007)
- Absolute difference of 18.3% (95% CI 5.7–30.9)
Authors’ Conclusions
- A larger trial is needed to confirm this potentially very beneficial effect of earlier surgery
- In the interim, there is a strong case for operating on patients with TICH who have a GCS of 9–12
- A strategy of early surgery is associated with a small, non-significant increase in health care costs
Strengths
- Relevant clinical question
- Randomised
- Multi-centre
- Outcome assessor blinded
- Intention-to-treat analysis
Weaknesses
- Internal Validity:
- Initial trial protocol published a priori but subsequently modified due to premature termination of trial and decreased sample size
- Temporal inclusion window from TBI increased from 24 h to 48 h during the trial to increase recruitment
- Large number of crossovers with a long time window from TBI to randomisation and significant departures from intended treatment
- Exploratory analyses of their effect on outcome and per treatment analyses currently unpublished
- 111 patients recruited from centres where screening logs were not collated
- Difficult to standardise clinical equipoise
- Dichotomised GOS used instead of ordinal GOSE analysis in primary outcome measure
- External Validity
- ICP monitoring only undertaken in 24 (14%) patients
- Underpowered study and only 4% of patients (6) recruited in the UK, most patients recruited from India and China with very different demographics and healthcare systems
- Secondary outcome measure of mortality likely to be multifactorial in aetiology and not as clinically relevant as morbidity in the context of TBI
- The secondary outcome analysis demonstrates a significant improvement in mortality offset by a non-significant increase in severely dependent patients
- The health care costs associated with a potential increase in severely dependent patients is not factored into the costing analysis
The Bottom Line
- Early surgery in TICH cannot be recommended solely on this evidence of a mortality benefit, a larger trial with a patient population generalisable to the UK is needed to explore if early surgery improves functional outcome in TICH
External Links
- [article] Early Surgery versus Initial Conservative Treatment in Patients with Traumatic Intracerebral Hemorrhage (STITCH[Trauma]): The First Randomized Trial
- [commentary] Traumatic Intracerebral Haemorrhage and Recruitment.
- [commentary] JC: A Stitch in Time
- [commentary] LITFL Research and Reviews in the Fastlane 089
Metadata
Summary author: @dramstewart
Summary date: 3 February 2016
Peer-review editor: @DuncanChambler





Pingback: Top 10+1 trauma papers 2016. St.Emlyn's - St.Emlyn's