TITRe2
TITRe2: Liberal or Restrictive Transfusion after Cardiac Surgery
Murphy. NEJM 2015;372(11):997-1008. doi:10.1056/NEJMoa1403612
Clinical Question
- In adults undergoing cardiac surgery, does a restrictive transfusion strategy (Hb > 75 g/l) compared to a liberal transfusion strategy (Hb > 90 g/l) lead to fewer infections and ischaemic events within 3 months?
Design
- Multi-centre, randomised, controlled trial
- Secure online allocation process with complete concealment
- Allocation minimisation to balance assignment by centre and surgery
- Clinicians not blinded, but patients and investigators were
- Patients were asked if they thought they knew their allocation at:
- discharge: 15.1% believed they did and 75.6% were correct
- 3 months: 27.5% believed they did and 56.6% were correct
- Patients were asked if they thought they knew their allocation at:
- Intention-to-treat analysis
- Power analysis concluded 1468 patients needed to have 90% power with two-sided 5% level of significance
- Increased to 2000 to allow for non-adherence
- Based upon estimate of primary outcome of:
- restrictive group 11%
- liberal group 17%
Setting
- 17 cardiac surgery centres across the UK
- July 2009 to February 2013
Population
- Inclusion: over 16 years undergoing non-emergency cardiac surgery
- Patients recruited and consented prior to surgery but only randomised and included if their Hb was recorded at below 90 g/l at any post-operative time
- Exclusion: patients unwilling to receive blood products (e.g. Jehovah’s Witnesses), congenital or acquired platelet, red cell or clotting disorders, sepsis, critical limb ischaemia, emergency surgery (occurring on same day as admission)
- 3565 consented, 2007 became anaemic and were randomised, 2003 analysed
Intervention
- Restrictive transfusion-threshold
- Threshold of 75 g/l
- 1 unit packed red cells transfused if threshold breached
- Repeated as needed if remained or dropped below 75 g/l again
Control
- Liberal transfusion-threshold
- Threshold of 90 g/dl
- 1 unit packed red cells transfused immediately after randomisation
- Repeated as needed if remained or dropped below 90 g/l again
Treatment common to both groups
- Treating physicians could contravene the assigned threshold and administer / withhold a transfusion, but only with clear documentation of the reason
- Treating physicians could permanently discontinue adherence to the assigned threshold
- Data were still collected as per intention-to-treat
- All other aspects of management were as per the treating centre’s usual care
Outcome
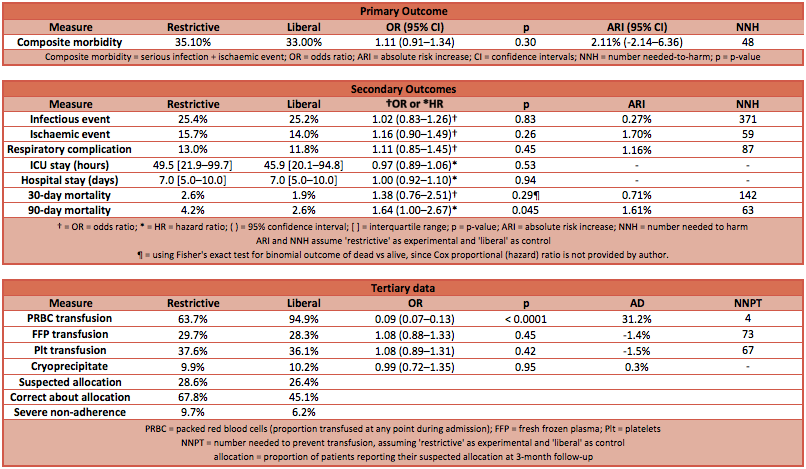
- Primary outcome: there was no statistically significant difference in the composite outcome of serious infections or ischaemic events within 3 months
- This outcome required the event to occur within the index hospital admission, or to have resulted in re-admission, or through detection by postal or phone survey of patients at home
- Restrictive transfusion group 35.1% vs Liberal transfusion group 33.0%
- Odds ratio 1.11 (95% CI 0.91 to 1.34); p-value 0.30
- Absolute risk increase 2.11% (95% CI -2.14% to 6.36%)
- Number needed to harm (by a restrictive transfusion practice) is 48
- Secondary outcome: the only secondary outcome (other than the dependent variable of red cell transfusions) to demonstrate a statistically significant difference was death at 90 days (according to a Cox proportional regression analysis) which favoured a liberal transfusion strategy
- Red cells transfused: liberal 95% vs restrictive 64%
- Number needed to prevent transfusion (by a restrictive transfusion practice) is 4
- Occurrence of infection: liberal 25% vs restrictive 25%
- Occurrence of an ischaemic event: liberal 14% vs restrictive 16%
- Median duration of ICU stay, HDU stay and hospital stay (see table)
- All cause mortality at 90 days: liberal 1.9% vs restrictive 2.6%
- p-value 0.045
- Number need to harm (by a restrictive transfusion practice) is 63
- Significant pulmonary complications: liberal 12% vs 13%
- EQ-5D health status: no statistical difference between groups or before and after surgery!
- Red cells transfused: liberal 95% vs restrictive 64%
- Tertiary data:
- Severe non-adherence to protocol: liberal 6.2% vs restrictive 9.7%
- Proportion of patients that suspected they knew their allocation at 3 months: liberal 26% vs restrictive 29%
- The proportion of these that were correct: liberal 45% vs restrictive 68%
Authors’ Conclusions
- The authors concluded that a restrictive transfusion strategy did not demonstrate clinical (or financial – data not presented here) superiority over a liberal transfusion strategy.
Strengths
- Important clinical question in a population not previous investigated through studies like TRICC, TRISS or Villanueva
- Patients in this trial had cardiovascular disease (although they were ‘treated’ for this during the index admission)
- Therefore, it might be reasonable to extrapolate these findings to unwell patients with cardiovascular disease (such as acute coronary syndrome)
- Very well planned and executed clinical research
- Attempts to blind pragmatically, and effort to investigate how successful this was
- Intention-to-treat, allowing clinicians to contravene allocation on clinical grounds
- Sensitivity analysis (data not presented here) investigated impact of this and found no significant effect on conclusion
- Considerable effort made to follow-up and detect outcome events in patients at home (leading to a rate double that of the anticipated rate)
- Transparent data available in detailed supplementary data
Weaknesses
- Composite outcome – can lead to clinically less significant but common outcomes being very influential on the conclusion, whilst clinically more significant but rarer outcomes are over-looked
- The secondary breakdown of events suggests this isn’t the case in this trial, since all sub-groups demonstrate little difference between the groups
- Un-blinding of patients – the difference in practice (give blood early vs give blood later) appears to have led to un-blinding of patients
- More patients in the restrictive group correctly identifying their allocation
- The authors attempted to collect objective outcomes using blinded assessors, limiting the bias that could occur if patients believed they knew (and correctly knew) their allocation
- The published supplementary data suggests that patients believed a liberal threshold was beneficial, thus the un-blinded restrictive-threshold patients may have biased their reporting of symptoms
- It is unclear exactly what impact, if any, this had on the conclusion
- It is likely that other trials have had this problem, but it has not been investigated or reported as succinctly as this trial has done so
- Number needed to prevent transfusion of 4 – although no clinical or financial differences were found in this trial, there are unmeasured consequences of transfusion
- If all measured factors are equal, a number needed to prevent transfusion of 4 may be very relevant to individuals who wish to avoid transfusion
- The only statistically significant difference was death at 90 days – if all other measured outcomes are almost equal, what is causing the difference in death at 90 days?
- More commonly, trials find a difference in morbidity but not in mortality, so this is an oddity
- Statistically, there is ~5% chance it is a false positive
- The authors suggest that the small numbers that died in this trial prevent a cause-and-effect conclusion being drawn, but that the trend is supportive of a theory that warrants further investigation
The Bottom Line
- In a group of patients with cardiovascular disease that have recently undergone cardiac surgery, a transfusion threshold of 75 g/l demonstrated no benefit over a transfusion threshold of 90 g/l
- There is possibly a trend towards increased morbidity, and an (unexplained) statistically significant increase in mortality from a 75 g/l transfusion threshold
- Global interpretation of this study is “in this group of patients, a transfusion threshold of 90 g/l is most appropriate”, but this RCT does not conclusively show this in my opinion
- It does suggest that clinicians are justified in tailoring transfusion thresholds of between 75 and 90 g/l to individual patients, as there is no definite harm and no cost difference (in the UK) from these two limits
External Links
- [article] TITRe2: Liberal or restrictive transfusion after cardiac surgery by Murphy et al
- [further reading] Post Cardiac Surgery Strategy: Liberal or restrictive transfusion? by ESICM
- [further reading] Transfusion Literature Summaries by LITFL
Metadata
Summary author: @DuncanChambler
Summary date: 8 April 2015
Peer-review editor: @SteveMathieu75