SETPOINT2

Effect of Early vs Standard Approach to Tracheostomy
on Functional Outcome at 6 Months Among Patients
With Severe Stroke Receiving Mechanical Ventilation:
The SETPOINT2 Randomized Clinical Trial
Bösel J. JAMA 2022; doi:10.1001/jama.2022.4798
Clinical Question
- In patients with severe stroke does early (≤5 days of intubation) tracheostomy when compared to standard timing (from day 10) of tracheostomy improve functional outcome at 6 months?
Background
- TRACMAN was one of the largest multi-centre RCTs looking at timing of tracheostomy in ICU
- The results did not provide any evidence supporting early tracheostomy
- The number of patients with a primary neurological reason for ICU admission were low (~5%) within this trial
- Rates of tracheostomy have been shown to be higher in those with acute brain injury compared to the general ICU population
- Concerns around weak cough, impaired swallow or an inability to maintain a patent upper airway often delay extubation in this population
- The SETPOINT trial looked at the timing of tracheostomy in stroke patients
- This small pilot RCT of 60 patients found no difference in ICU LOS (the primary outcome) but did show a lower ICU mortality (a secondary outcome)
Design
- Investigator initiated, multi-centre, randomised trial
- Blinding of outcome assessors (long term functional and cause of mortality)
- Outcomes assessed using pre-structured telephone interview
- Informed consent by patient or their legally authorised representative prior to day 4 of intubation
- Randomised in 1:1 ratio
- Central web-based tool
- Blocks stratified in groups of 4 to achieve equal group size per centre
- Only centres with routine use of percutaneous dilatational tracheostomy (PDT) were recruited
- Sample sized based on pilot trial
- 15% increase from 30% to 45% in intervention group
- With 80% power and alpha of 0.05 and 15% drop out rate a sample size of 380 (190 per group was required)
- Pre-specified subgroups
- Confidence intervals for secondary end-points and subgroups not adjusted for multiplicity
- Thus, these can only be interpreted as exploratory
- Missing values for mRS at 6 months handled by a multiple imputation approach
- Appropriate ethical approval
- Registered with Clinical Trials
Setting
- 26 neurocritical care units in Germany and USA
- July 2015 – August 2020
Population
- Inclusion:
- 18 years or older
- Invasive mechanical ventilation (IMV)
- Acute ischemic stroke (AIS), intracerebral haemorrhage (ICH) or sub arachnoid haemorrhage (SAH) (all non traumatic)
- SETscore > 10
- Predicts the need for IMV for at least 2 weeks
- Calculated on day of enrolment
- Clinical judgement of treating neuro-intensivist that tracheostomy likely to be needed
- Principle indication for tracheostomy had to be at least one of:
- Ongoing demand for suctioning secretions
- CNS related respiratory insufficiency
- aspiration or danger of aspiration due to dysphagia
- Exclusion:
- mRS > 1 (pre-morbid)
- IMV > 4 days
- Clinical conditions prohibiting early tracheostomy or mandating surgical tracheostomy
- Pregnancy
- Life expectancy < 3 weeks
- Anticipated withdrawal of life sustaining therapies
- Inability to obtain informed consent
- Participation in other interventional trial
- 4562 assessed for eligibility –> 4180 excluded for not meeting eligibility criteria
- 188 randomised to early tracheostomy –> 177 had tracheostomy (95.2%)
- 177 in primary analysis as 9 lost to follow up and 2 withdrew consent
- 194 randomised to late tracheostomy –> 130 had tracheostomy (67%)
- 189 in primary analysis as 4 lost to follow up and 1 withdrew consent
- 188 randomised to early tracheostomy –> 177 had tracheostomy (95.2%)
- Comparing baseline characteristics (early vs. standard tracheostomy groups):
- Age: 59.2 vs 57.6
- Male: 48.4% vs 52.1%
- Pre-hospital mRS of 0: 86.0% vs 87.1 %
- Admission:
- Median NIHSS: 21 vs 21
- Median GCS: 7 vs 6
- Median SETscore: 14 vs 14
- Diagnosis:
- AIS: 26.3% vs 30.4%
- Decompressive Craniectomy: 49.0% vs 50.8%
- ICH: 41.9% vs 40.2%
- Volume > 30cc: 60.5% vs 71.8%
- Supratentorial: 71.8% vs 75.6%
- SAH: 31.7% vs 29.4%
- WFNS Score: 5 vs 5
- Fisher Scale of 4: 67.2% vs 73.7%
- AIS: 26.3% vs 30.4%
- Baseline Lung Injury Score: 1.0 vs 1.0
- PDT (if tracheostomy performed): 89.3% vs 83.1%
- Time from intubation: 4 days vs 11 days
Intervention
- PDT within 5 days of IMV
Control
- PDT after 10 days of IMV
Management common to both groups
- Conversion to surgical tracheostomy allowed if clinically warranted
- All other management (including ventilator settings, weaning, analgesia and sedation) centre specific but followed guidelines from American Heart and Stoke Associations and Neurocritical Care Society
Outcome
- Primary outcome:
- mRS of 0 – 4 or less at 6 months
- 43.5% in early group vs 47.1% in standard group
- Absolute difference -3.6% (95% CI -14.3 to 7.2%)
- aOR 0.93 (95% CI 0.60 to 1.42)
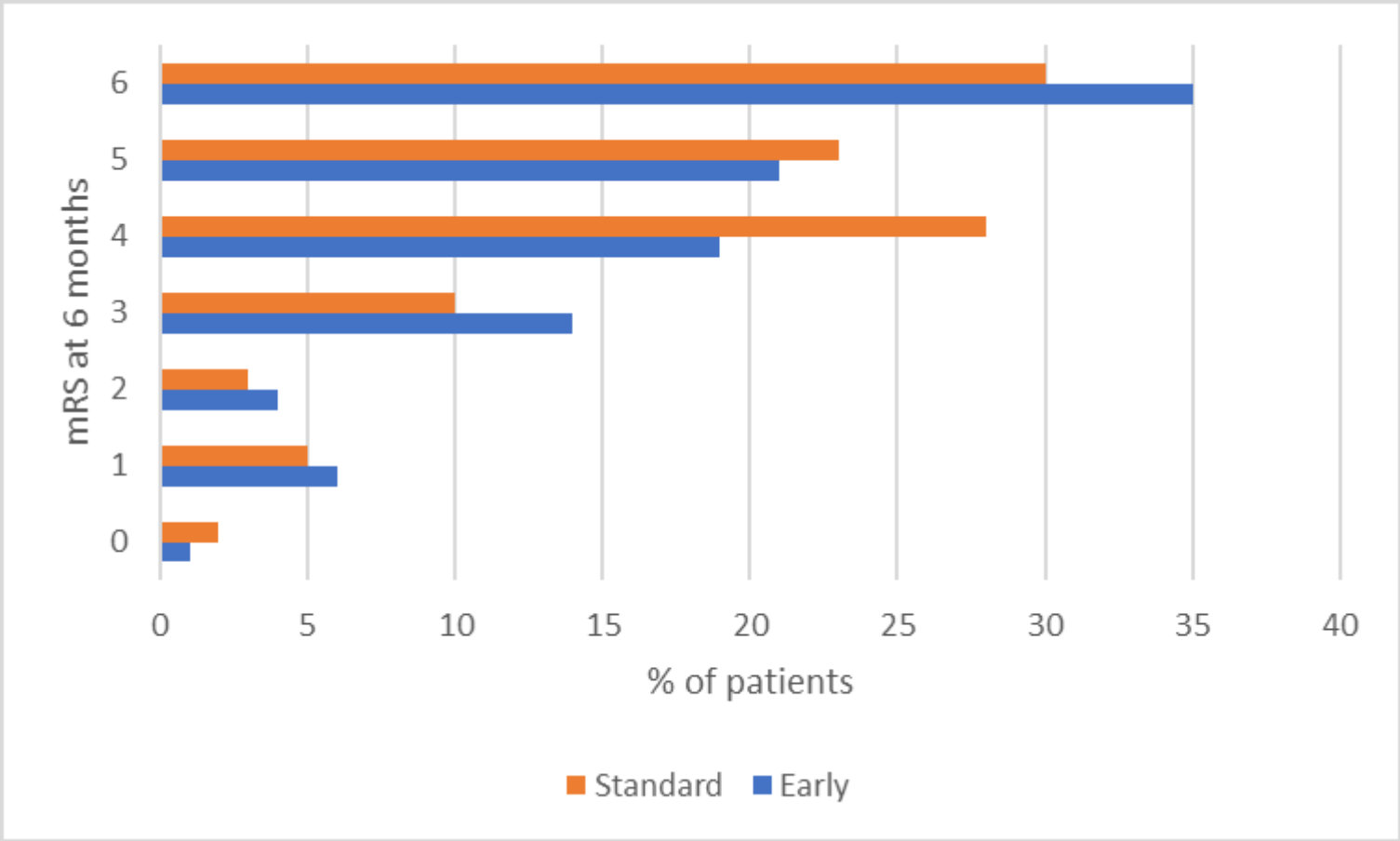
- Secondary outcomes:
- Comparing early vs. standard group
- No secondary outcome showed a significant difference
- mRS 0 – 3 at 6 months
- 24.3% vs 19.6%
- aOR 1.48 (95% CI 0.89 – 2.48)
- 24.3% vs 19.6%
- Death at 6 months
- 35.0% vs 29.6%
- aOR 1.06 (95% CI 0.74 – 1.53)
- 35.0% vs 29.6%
- Median time to ICU discharge
- 17 days vs 19 days
- HR 1.12 (95% CI 0.90 – 1.39)
- 17 days vs 19 days
- Median time to end mechanical ventilation
- 14 days vs 11 days
- HR 0.97 (0.73 to 1.31)
- 14 days vs 11 days
- No difference in ICU stay without sedatives, opioids or vasopressors
- mRS 0 – 3 at 6 months
- No secondary outcome showed a significant difference
- Subgroups:
- No subgroup had 95% CI that fully favoured one approach or other
- These included Age (< 55, 55 – 65, > 65), Sex, Location (USA or Germany), Recruitment Numbers (<30 or > 30), Primary diagnosis (AIS, SAH or ICH), and GCS (<6, ≥6)
- Safety Outcomes
- (potentially) PDT related adverse event rate 17.3% (eTable 5)
- 16.9% vs 17.7%
- Periprocedural adverse events (up to 2 hours post tracheostomy): 15.8%
- Any serious adverse event:
- 47.3% vs 43.8%
- (potentially) PDT related adverse event rate 17.3% (eTable 5)
Authors’ Conclusions
- In patients with severe stroke receiving IMV, early tracheostomy did not improve rate of survival without significant disability at 6 months compared to standard timing
- Clinically relevant benefit or harm can not be excluded due to wide confidence intervals
Strengths
- Multi centre RCT across 2 countries increase external validity
- Although 4130 were excluded, an accurate screening log minimises selection bias and shows that a majority were excluded for valid reasons (not meeting inclusion criteria or meeting exclusion criteria)
- Only 1.3% (n=55) were excluded for “other” reasons
- Analysed on intention to treat basis
- Balanced baseline characteristics
- Achieved a meaningful separation in timing of tracheostomy
- Good adherence to protocol – no violations reported
- Minimal loss to follow up (3.4%)
Weaknesses
- The primary outcome of an mRS of 0-4 ranges from no disability to moderate severe disability that requires the assistance of others for mobility and daily needs
- This is a very wide range of functional outcomes. One wonders if a patient who has an mRS of 4 would view this as a “better” functional outcome?
- Secondary end-points regarding ICU medications were defined post-hoc
- Understandably unable to blind clinicians and patients
- No standardised weaning protocol used
- 48.7% of all randomisations came from 4 centres (2 in USA, 2 in Germany)
- 33% of standard tracheostomy group did not receive a tracheostomy
- 22% were extubated and 11% died prior
- This confirms prior studies about the utility of the SETscore and its ability to predict those that will be extubated successfully in the short term
- However, over 1 in 5 patients did not have a procedure that had a near 20% complication rate
- AIS, ICH and SAH may have different clinical courses
- ICH may have worse functional prognosis than AIS in retrospective studies
- This appeared to be a cohort that had a poor prognosis (evidenced by high decompressive craniectomy rates, and high WFNS scores)
- This is also evident in the fact that only ~10% in each group had a mRS of 0-2
- Would a difference be shown if the cohort was less likely to have an unfavourable outcome?
The Bottom Line
- This trial provides no evidence that in patients with severe stroke an early tracheostomy is better than standard time for tracheostomy, and that an early tracheostomy may mean a patient has to undergo a procedure that they did not need
External Links
- [article] SETPOINT2
- [further reading] Early vs Late Tracheostomy in ICU patients: a meta analysis of randomised controlled trials
Metadata
Summary author: George Walker @hgmwalker89
Summary date: 13th May 2022
Peer-review editor: @davidslessor
Picture by: iStock



