Endovascular Therapy for Large Ischemic Stroke
Endovascular Therapy for Acute Stroke with a Large
Ischemic Region
S. Yoshimura. NEJM 2022; 386:1303-1313. doi:10.1056/NEJMoa2118191
Clinical Question
- In patients with large cerebral infarction volumes does the use of endovascular therapy alongside medical care compared with medical care alone improve 90-day functional outcomes?
Background
- Endovascular treatment (EVT) of acute stroke caused by the occlusion of large vessels has been proven to be a highly effective treatment that reduces death and disability
- This has been proven in multiple trials (MR CLEAN, DAWN, EXTEND-IA, DEFUSE III, SWIFT PRIME)
- The ASPECTS score is a semi-quantitive score to characterise the extent of middle cerebral artery (MCA) stroke
- It ranges from 10 to 0, where 0 indicates the largest infarct burden
- Previous trials have excluded (or have limited numbers of) those with larger infarct volumes due to concerns surrounding risk of bleeding following reperfusion
- A systematic review looking at those with a larger infarct volume (ASPECTS < 6 or core volume > 50 cc) found no risk of increased haemorrhage and improved functional outcomes with the use of EVT
Design
- Open-label, parallel-group, RCT
- Central randomisation in a 1:1 ratio
- Algorithm used to balance trial group assignments within hospitals on basis of age, interval between last known well and arrival, NIHSS score on admission, and use of rt-PA
- Assignments not concealed from patients or treating physicians
- Trained assessors of mRS blinded
- Clinical assessments performed at baseline and then 12 hours, 24 – 72 hours, 5 – 9 days and 60 – 120 days after randomisation
- Power calculation based on local registry data, which showed an aOR of 3.42 in favour of EVT
- Given this was observational registry data the authors assumed an adjusted OR of 2.7 (20% less than observed)
- This required 81 in each arm, which was increased to 200 in total to allow for 15% drop out and withdrawal of consent (90% power with two-sided alpha of 0.05)
- Primary analysis performed on all those randomised and had assessable outcome data
- Event adjudication (assessing the mRS scores used for randomisation) and imaging committees (assessing the imaging used for randomisation) could remove patients from trial if clinical or imaging parameters used for inclusion were not met on review
- A per-protocol analysis performed on those not excluded
- Pre-specified subgroups
- The subgroup for time last known well was added post-hoc
- Written informed consent provided prior to enrolment
Setting
- Japan, 45 hospitals
- November 2018 – September 2021
Population
- Inclusion:
- > 18 years old
- NIHSS score of at least 6
- a pre-morbid mRS of 0 or 1
- Internal carotid or M1 segment of middle cerebral artery occlusion on CTA/MRA
- ASPECTS score 3 – 5
- Within 6 hours of last known well or if within 6 – 24 hours then FLAIR sequence on MRI had to show recent infarct
- EVT initiated within 60 minutes following randomisation
- Exclusion:
- Clinically significant mass effect with midline shift
- Acute intracranial haemorrhage
- Pregnant or suspected pregnancy
- Evidence of chronic occlusion
- Investigators felt high risk of haemorrhage (Plts < 40, APTT > 50, INR > 3)
- Judged to likely be non-compliant or uncooperative
- 235 assessed for eligibility –> 203 randomised
- 100 in EVT group (6 excluded after adjudication) –> 94 per protocol
- 102 in medical group (8 excluded) –> 94 per protocol
- Across both arms, 11/14 removed were for ASPECTS score other than 3 to 5 or no presence of ICA or M1 occlusion
- Comparing baseline characteristics of EVT vs. Medical Care group
- Generally similar although larger infarct volume in Medical Care
- Age: 76.6 vs 75.7
- Male: 54.5% vs 56.9%
- Medical History:
- Hypertension: 70.3% vs 68.6%
- AF: 59.4% vs 58.8%
- Systolic BP: 156 mmHg vs 163 mmHg
- Median mRS prior: 0 vs 0
- Median NIHSS at baseline: 22 vs 22
- Median ASPECTS: 3 vs 4
- Median Infarction Volume: 94ml vs 110mls
- IV rt-PA use: 26.7% vs 28.4%
- Median time between stroke onset and hospital arrival: 190 mins vs 170 mins
- Median time between stroke onset and randomisation: 229 mins vs 214 mins
- For those in EVT group:
- Median time between stroke onset and reperfusion: 308 mins
- TICI >/= 2b: 86%
Intervention
- Endovascular Therapy and Medical Care
- EVT method selected by treating physicians (could include stent retriever, aspiration catheter, balloon angioplasty, intracranial or carotid stent)
- 98% had thrombectomy
- Success defined as TICI2b (anterograde reperfusion of > 50% of previously occluded territory)
- EVT method selected by treating physicians (could include stent retriever, aspiration catheter, balloon angioplasty, intracranial or carotid stent)
Control
- Medical Care only
Management common to both groups
- rt-tPA allowed (0.6mg/kg) as per Japanese guidelines and at discretion of treating physician
- Medical Care was as per the AHA and American Stroke Association guidelines
Outcome
- Primary outcome (mRS of 0-3 at 90 days)
- Comparing EVT vs Medical Care
- 31% vs 12.7%
- Relative Risk 2.43 (95% CI 1.35 – 4.37), p = 0.002
- ARR 18.3% (95% CI 7.1 – 18.3%)
- NNT 6 (95% CI 3.4 – 14.1)
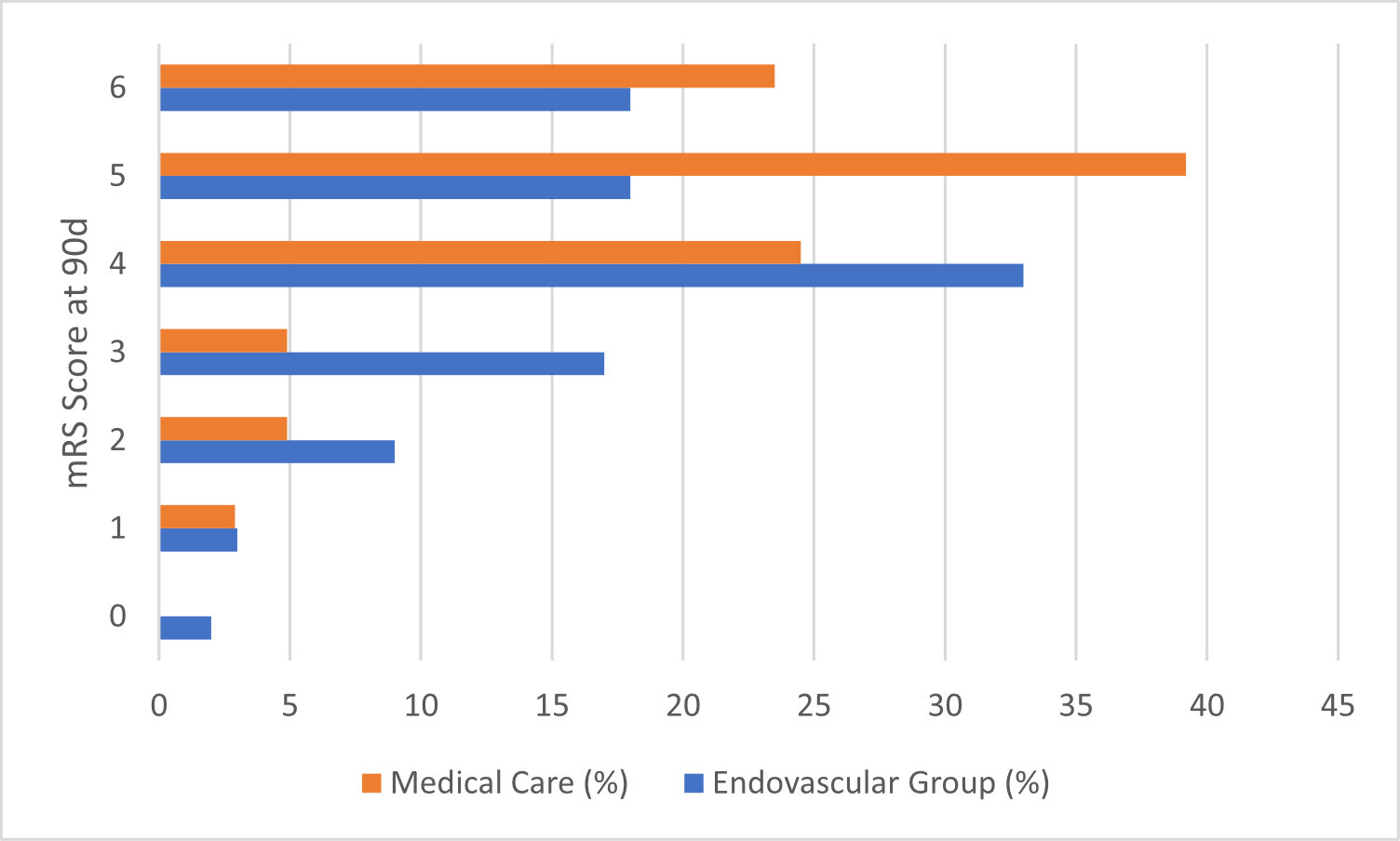
- Secondary outcomes:
- Comparing EVT vs. Medical Care group
- No significant difference in
- mRS of 0-2 at 90 days
- 14.0% vs 7.8% (RR 1.79, 95% CI 0.78 – 4.07)
- mRS of 0 or 1 at 90 days
- 5.0% vs 2.9% (RR 1.70, 95% CI 0.42 – 6.93)
- mRS of 0-2 at 90 days
- Significantly greater in intervention group
- Ordinal shift in mRS towards better outcome
- RR 2.42 (95% CI 1.46 – 4.01)
- Improvement in ≥8 points on the NIHSS at 48 hr
- 31.0% vs 8.8% (RR 3.51, 95% CI 1.76 – 7.00)
- Ordinal shift in mRS towards better outcome
- No significant difference in
- Selected Subgroups
- All point estimates favoured EVT
- The following subgroups had 95% CI that fully favoured EVT:
- Age ≥ 75: RR 3.05 (95% CI 1.19 – 7.85)
- Interval between last known well and randomisation < 6 hrs: RR 2.43 (95% CI 1.25 – 4.74)
- No use of rt-PA: RR 2.52 (1.25 – 5.07)
- Safety Outcomes
- Higher rates of any intracranial haemorrhage (ICH) within 48 hours
- 58.0% vs 31.4% (RR 1.85, 95% CI 1.33 – 2.58, p < 0.001)
- However, rates of symptomatic ICH rates similar
- 9.0% vs 4.9% (RR 1.84, 95% CI 0.64 – 5.29, p = 0.25)
- Other safety outcomes including death within 90 days, recurrence of infarction within 90 days or decompressive craniectomy within 7 days were all similar
- Procedural complication rate: 8.9%
- 5% vessel perforation
- Other serious AE:
- 33.7% in EVT group compared to 18.6% in Medical Care
- Higher rates of any intracranial haemorrhage (ICH) within 48 hours
- The results of the per-protocol analysis was similar to the results described above
Authors’ Conclusions
- Amongst patients in Japan with an acute stroke and large ischaemic region functional outcomes at 90 days were better with endovascular therapy and medical care compared to medical care alone
- Endovascular therapy was associated with a higher incidence of intracranial haemorrhage
Strengths
- Randomised trial answering an important clinical question in area of medicine that has a large evidence base for its use
- Generally balanced baseline characteristics
- Analysed on an intention to treat basis
- Of all those that were randomised only 1 patient in the EVT group withdrew consent and as such was not included in the analysis
- No loss to follow up documented
- No cross-over reported
- Trained and blinded assessors of primary outcome
- The infarct volume was larger than in other trials:
- For DAWN the infarct volume had to be < 50ml, for DEFUSE III < 70ml and median ASPECTS score of 9 in SWIFT PRIME
Weaknesses
- Single country setting may limit external validity
- Only 6/45 centres had ≥ 10 participants and 20/25 had ≤ 3 (average 1/yr)
- This maybe important with regards to the lower volume centres and complication rates
- mRS only rates physical ability but no other QoL metrics were reported which would no doubt be important to the patient
- High rates of cognitive impairment have been demonstrated post ischaemic stroke
- Slight but potentially clinically important change in primary outcome compared to other comparator trials
- DEFUSE III, EXTEND IA, SWIFT PRIME all used an mRS score of 0-2 as the primary outcome
- An mRS of 2 is slight disability whereas 3 is moderate disability with the requirement with some assistance
- There was no difference between groups for an mRS of 0-2 at 90d
- Although the ASPECTS score were higher in the medical group (better) the stroke volume was larger by 16 ml
- Initial approach to imaging may not be consistent with other countries initial radiological assessment of stroke in the ED:
- High rates of MRI (88%) as opposed to CT to determine ASPECTS score
- MRI has been shown to have lower ASPECT scores compared with CT
- No use of perfusion imaging to guide treatment
- This may help better determine salvageable tissue
- High rates of MRI (88%) as opposed to CT to determine ASPECTS score
- Low rates of rt-PA use compared to other countries (and lower doses)
- Higher rates of rt-PA may improve the outcomes in the medical care group
- Funded by Mihara Cerebrovascular Disorder Research Promotion Fund and Japanese Society for Neuro-Endovascular Therapy
- Both non-profit and had no role in any design or conduct of the trial
The Bottom Line
- Following this trial it will be important to discuss the use of EVT in large ischaemic strokes
- However, any decision will need to be made in a multi-disciplinary approach given some concerns around external generalisability, the higher rates of intracranial haemorrhage and serious adverse events alongside the fact a large number of patients still have significant disability
External Links
- [article] Endovascular Therapy for Acute Stroke with a Large Ischemic Region
- [editorial] In Stroke, When is a Good Outcome Good Enough?
Metadata
Summary author: George Walker @hgmwalker89
Summary date: 12th May 2022
Peer-review editor: Dave Slessor
Picture by: iStock / wildpixel





Such a great blog! Thank you for this information, I appreciate your effort, please keep us update.
Thank you so much, truly grateful for the info.