TOMAHAWK
Angiography after Out-of-Hospital Cardiac Arrest without ST-Segment Elevation
Desch S et al. NEJM 2021. DOI: 10.1056/NEJMoa2101909
Clinical Question
- In adults > 30 years old suffering out-of-hospital cardiac arrest (OOHCA) without ST elevation on their ECG does routine immediate coronary angiography compared to a delayed or selective approach to coronary angiography improve 30-day all-cause mortality?
Background
- The DISCO pilot study showed that in this cohort of patients a culprit lesion was found in ~37% of those undergoing immediate coronary angiography
- A culprit lesion was defined as a stenosis > 50%
- 2021 ERC guidelines currently suggest that emergent coronary angiography should be considered if there is high clinical suspicion of a coronary artery occlusion (e.g. haemodynamic compromise / electrical instability)
- This is a subtle change from the 2015 guidelines
- This was based on the COACT trial
- This trial found in those with an initial shockable rhythm without ST elevation on their ECG that immediate coronary angiography did not improve 90-day mortality
Design
- Investigator initiated, randomised, multi-centre, open-label trial
- Screened for eligibility on ED arrival
- If eligibility criteria met, then randomised in 1:1 ratio using a web-based system
- Randomly changing block sizes used
- Primary outcome was all cause mortality at 30 days
- Multiple pre-specified secondary end points and pre-specified subgroup analyses
- Power calculations based on 2012 registry study which showed 30-day mortality 34% in immediate angiography vs. 46% in delayed angiography
- Parameters for calculation provided in supplementary appendix
- 558 patients were calculated to provide 80% power to reject the null hypothesis of no difference
- Interim analysis planned after 109 events
- Primary analysis performed on an ITT basis
- A sensitivity analysis was performed with a per-protocol analysis, and safety analyses performed according to those treated
- Appropriate consent process (described in supplementary appendix)
- Registered with ClinicalTrials.gov NCT02750462
Setting
- 31 sites in Germany and Denmark
- November 2016 – September 2019
Population
- Inclusion:
- Adults > 30 years
- Resuscitated OOHCA (both shockable and non-shockable rhythms)
- Informed consent
- Exclusion:
- ST-segment elevation or LBBB
- No ROSC on hospital admission
- Severe haemodynamic or electrical instability
- Clinical criteria for haemodynamic instability were initially provided, however for the final study protocol these were removed and the decision was left to the discretion of the treating clinician
- Obvious extra-cardiac cause (e.g. TBI, drowning etc)
- In-hospital cardiac arrest
- Pregnancy (known or suspected)
- Participation in another trial interfering with the research questions of TOMAHAWK
- 558 patients eligible ➝ 554 randomised (4 not randomised due to technical reasons)
- 281 ➝ Immediate angiography ➝ 265 analysed
- 273 ➝ Delayed / Selective angiography ➝ 265 analysed
- Generally balanced baseline characteristics (Immediate vs. Delayed / Selective) – slightly higher rates of smoking, coronary artery disease and shockable initial rhythm in delayed group
- Baseline Demographics
- Age: 69 v 71
- Female Sex: 30.2% vs 30.6%
- BMI: 26.5 vs 26.2
- Diabetes: 29.1% vs 29.5%
- Hypertension: 67.1% vs 69.2%
- Current Smoker: 29.9% vs 34.5%
- Coronary Artery Disease: 34.5% vs 40.6%
- Prior MI: 19.3% vs 19.8%
- Prior PCI: 18.4% vs 16.4%
- Prior CABG: 8% vs 10.6%
- Cardiac Arrest Demographics
- Witnessed Arrest: 91.1% vs 87.9%
- Shockable initial rhythm: 52.3% vs 58.7%
- Bystander CPR: 57.5% vs 60.3%
- Median time from arrest to basic life support: 2 vs 1 min
- Median time to ROSC: 15 vs 15 mins
- Hospital Admission Parameters (all median):
- GCS: 3 vs 3
- SBP: 110 vs 110
- LVEF (%): 45 vs 44
- Lactate: 5 vs 4.9
- Creatinine: 118 vs 111
- Trop T: 0.09 vs 0.08 μg/L
- Trop I: 0.4 vs 0.1 μg/L
- Coronary Angiography
- Angiography performed: 95.5% vs 62.2%
- Median time from arrest until angiography: 2.9 vs 46.9 hrs
- Culprit Lesion: 38.1 vs 43.0%
- PCI performed: 37.2% vs 43.2%
- Baseline Demographics
Intervention
- Immediate angiography
- Transferred to cath lab ASAP
Control
- Delayed / Selective angiography
- Transferred to ICU for further evaluation
- If likelihood of an acute coronary trigger was high (based on examination and testing at discretion of treating physician) then could proceed to angiography with a minimum of a 24 hour delay
- Criteria for angiography prior to 24 hour delay included:
- Substantial myocardial damage (cardiac troponin >70x ULN or increase in CK 10x ULN at least 6 hours post arrest)
- Electrical instability
- Cardiogenic shock
- New ST-segment elevation
- If clinical examination and testing suggested that cardiac cause unlikely then angiography could be further delayed or abandoned
Management common to both groups
- Revascularisation attempted if at least 1 major coronary artery had disease that was deemed to be clinically relevant
- Ideally this was PCI as opposed to CABG, but decision at discretion of treating teams
- Other post-resuscitation care was as provided as per the local standard
Outcome
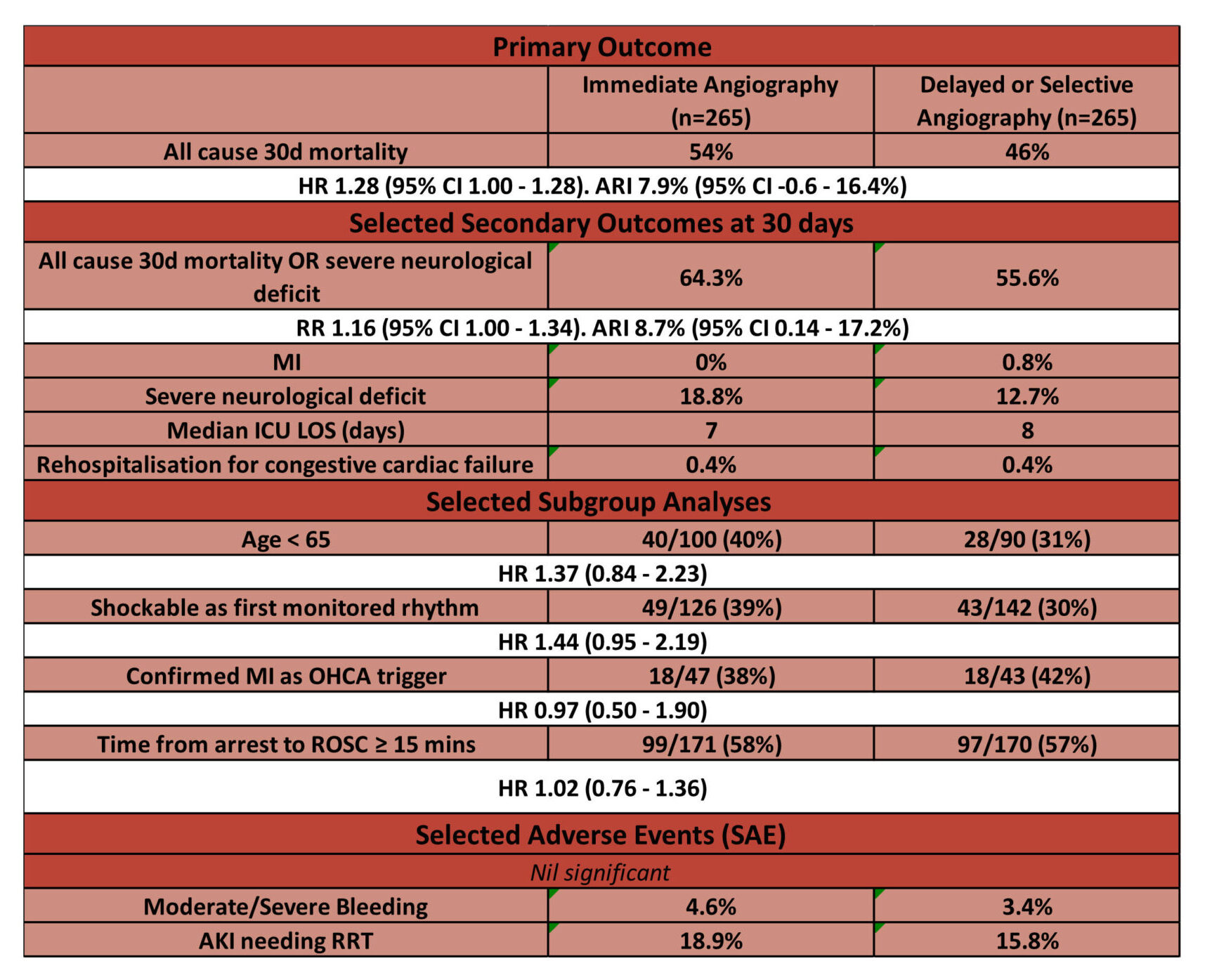
- Primary outcome: 30d risk of death from any cause – no significant difference
- Immediate Angiography vs. Delayed / Selective Angiography
- 54 vs 46%
- HR 1.28 (95% CI 1.00 – 1.63)
- Immediate Angiography vs. Delayed / Selective Angiography
- Secondary outcome and safety outcomes:
- Comparing Immediate Angiography vs. Delayed / Selective Angiography
- Secondary outcomes not adjusted for multiplicity – therefore may not be reproducible.
- 30d Death from any cause or severe neurological deficit: 64.3% vs. 55.6%
- [RR 1.16 (95% CI 1.00 – 1.34)]
- 30d Myocardial Infarction: 0% vs 0.8%
- 30d Severe Neurological Deficit: 18.8% vs 12.7%
- Defined as CPC 3 – 5
- Median ICU LOS: 7 vs 8 days
- 30d Re-hospitalisation for congestive cardiac failure: 0.4% vs 0.4%
- Median peak release of cardiac enzymes:
- Trop T: 0.39 vs 0.34 μg/L
- Trop I: 1.46 vs 1.10 μg/L
- Median peak creatinine: 133 μmol/L vs 133 μmol/L
- 30d Moderate / Severe bleeding: 4.6% vs. 3.4%
- 30d Stroke: 1.6% vs. 2.1%
- 30d AKI leading to RRT: 18.9% vs. 15.8%
- 30d Death from any cause or severe neurological deficit: 64.3% vs. 55.6%
Authors’ Conclusions
- In resuscitated patients with a possible cardiac cause of OOHCA without ST elevation or LBBB an immediate coronary angiography strategy did not reduce 30 day risk of death from any cause compared to a delayed or selective coronary angiography strategy
Strengths
- Good randomisation process with randomly changing block size and sensible inclusion and exclusion criteria
- Balanced baseline characteristics
- Primary outcome patient focused
- All end-points clearly defined, thus minimising variability between outcome assessors
- Pre-specified secondary outcomes, safety outcomes and subgroups
- Multi-centre trial across two European countries increases external validity
- Primary outcome performed on an ITT basis
- Findings correlate with COACT trial
Weaknesses
- Despite only 4 of those who were eligible not being randomised, a screening log was only collected at the very beginning of the trial
- This may introduce an unrecognised selection bias as there is no record as to why potentially eligible patients are not enrolled
- Many would advocate for immediate angiography if an OOHCA patient with a potential cardiac cause was haemodynamically unstable or in cardiogenic shock
- This exclusion criteria was changed from initially having a set of criteria to being solely at the clinical discretion of treating physician.
- It is unclear as to the degree of haemodynamic instability for which patients were excluded.
- This makes it harder to fully understand the haemodynamic characteristics of patients involved.
- Unblinded
- Understandable that treating staff not blinded but no mention that trial members not involved in clinical management were blinded
- The 12% absolute difference in 30-day mortality that the power calculations were based on seems high
- The authors acknowledge this is based the minimal available data at the time of study planning. However, the exclusion of high risk patients who are likely to benefit from immediate PCI (e.g. haemodynamic or electrical instability) means that a 12% absolute difference between groups is potentially optimistic
- 95% CI for secondary outcomes are not adjusted for multiplicity
- This means inferences drawn from these may not be reproducible, so as the authors rightly state, the secondary outcome are hypothesis generating only
- High rates of cross-over from delayed / selective strategy ➝ coronary angiography < 24 hours
- 46 patients (17%)
- 24 of these were for permitted reasons (11 cardiogenic shock, 6 Large myocardial injury, 5 new ST-Elevation, 2 electrical instability)
- 22 of these violated study protocol
- 46 patients (17%)
- Currently the published follow-up is only to 30 days, longer term follow up (which is planned) may reveal some clinically important differences between groups e.g. LV function
The Bottom Line
- For patients presenting with a suspected cardiac cause of OOHCA who are haemodynamically stable, there appears to be no benefit from immediate angiography
- As such, admission to the ICU for ongoing stabilisation and investigation is a reasonable initial management strategy for this group of patients
- For patients with haemodynamic compromise or electrical instability I will continue to discuss with cardiology about optimal timing for angiography
- Further trials such as ARREST and DISCO will continue to inform practice
External Links
- [paper] TOMAHAWK trial
- [further reading] 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
Metadata
Summary author: George Walker @hgmwalker89
Summary date: 2nd September 2021
Peer-review editor: David Slessor
Image by: iStock



