VITdAL-ICU

VITdAL-ICU: Effect of High-Dose Vitamin D3 on Hospital Length of Stay in Critically Ill Patients with Vitamin D Deficiency
Amrein. JAMA 2014; 312:1520-30. doi:10.1001/jama.2014.13204
Clinical Question
- In critically ill patients with low serum vitamin D levels, does high-dose vitamin D supplementation compared with placebo reduce hospital length of stay?
Design
- Randomised, controlled trial
- Computerised randomisation in blocks of 8, stratified according to ICU type and sex
- Fully blinded: patients, clinicians and assessors
- Intention-to-treat analysis
- Powered at 80% to detect a reduction in hospital stay by 2 days from a baseline of 14 days (standard deviation 7 days) with a significance level defined at 0.05
- Allowed for 5% drop-out rate
- Required 490 patients
Setting
- Single-centre with five different ICUs: medical, neurological, cardiothoracic and two mixed-surgical
- Based in tertiary academic centre in Austria
- May 2010 to March 2012
Population
- Inclusion: over 18 years, expected to stay in ICU for 48 hours or more, 25-hydroxyvitamin D < 20 ng/ml (49.92 nmol/l)
- Exclusion: gastrointestinal failure, pregnant or lactating women, hypercalcaemia (total calcium > 10.6 mg/dl [2.65 mmol/l] or ionised Ca2+ > 5.4 mg/dl [1.35 mmol/l]), diagnosis of TB, sarcoidosis or kidney stones in past year
- 1140 assessed, 492 recruited and 475 included in analysis (12 did not receive assigned medication, 5 withdrew consent)
- Baseline characteristics (Placebo vs Vitamin D3)
- Mean age in years: 65.3 vs 63.9
- Ethnicity: 100% white vs 100% white
- BMI: 27.1 vs 27.2
Intervention
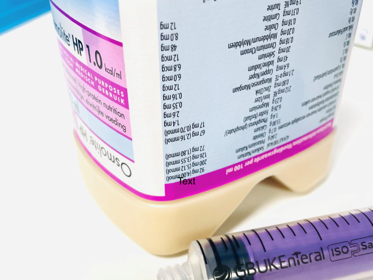
- Vitamin D (Oleovit D3, Fresenius Kabi)
- Loading dose of 540,000 IU vitamin D in 45 ml oleum arachidis orally or via nasogastric tube
- Maintenance dose of 90,000 IU vitamin D in 7.5 ml oleum arachidis monthly from day 28 for five months
- Standard vitamin D supplementation of 200 IU per day could be given at physicians discretion
- Patients were requested to avoid other vitamin D supplements
Control
- Placebo (identical color, smell and taste)
- Loading dose of 45 ml oleum arachidis
- Maintenance dose 7.5 ml oleum arachidis monthly from day 28 for five months
- Standard vitamin D supplementation of 200 IU per day could be given at physicians discretion
- Patients were requested to avoid other vitamin D supplements
Outcome
- Primary outcome: hospital length of stay was not statistically different between the groups (comparison as median days with interquartile range)
- Vitamin D: 20.1 days (11.1 to 33.3)
- Placebo: 19.3 days (11.1 to 34.9)
- p value = 0.98
- Secondary outcome: there were no statistically different outcomes, but the trend favoured the vitamin D group (comparison is placebo vs vitamin D, hazard ratio with 95% confidence intervals and p-values)
- ICU length of stay: 10.7 days vs 9.6 days; p=0.38
- ICU mortality: 26.5 vs 22.8; HR 0.97 (0.67–1.39); p=0.86
- 28-day mortality: 28.6 vs 21.9; HR 0.76 (0.53–1.09); p=0.14
- Hospital mortality: 35.3 vs 28.3; HR 0.81 (0.58–1.11); p=0.18
- 6-month mortality: 42.9 vs 35.0; HR 0.78 (0.58–1.04); p=0.09
- Subgroup analysis: in the subgroup of severe vitamin D deficiency (≤12 ng/ml), both the effect size and point accuracy increased, with statistical significant benefit of vitamin D at 28-day, hospital and 6-month mortality.
Authors’ Conclusions
- “Among patients with vitamin D deficiency who are critically ill, administration of high-dose vitamin D3 compared with placebo did not improve hospital length of stay, hospital mortality, or 6-month mortality”
Strengths
- Well designed, randomised, controlled trial with appropriate concealment, blinding and statistical analysis – strong internal validity
- Full recruitment for planned statistical power, with no loss-to-follow-up and minimal withdrawal
- Mixed ICU population
Weaknesses
- Choice of primary outcome (length of stay) is less relevant than mortality, but the authors justify this weakness: no pilot data available to base power calculation on
- Strong emphasis on subgroup outcomes, but authors suggest this should be hypothesis generating and not conclusive evidence
- No representation of non-white, non-adult populations limiting external validity
- Small sample size may not allow detection of rare but significant side effects
The Bottom Line
- This well designed trial suggests that severe vitamin D deficiency in critically ill patients may benefit from high-dose supplementation, but as a single-centre and relatively small trial the findings need to be validated by further trials before a treatment recommendation can be made
External Links
- [article] VITdAL-ICU: Effect of High-Dose Vitamin D3 on Hospital Length of Stay in Critically Ill Patients with Vitamin D Deficiency
- [podcast] Interview with Karin Amrein (trial author) by Intensive Care Network
- [further reading] Vitamin D in Critical Care by LITFL
- [blog] Conference notes from Critical Care Reviews 2015, including presentation of this study by Karin Amrein
Metadata
Summary author: @DuncanChambler
Summary date: 28 January 2015
Peer-review editor: @stevemathieu75



Pingback: VIOLET – The Bottom Line