iPROVE
Individualised perioperative open-lung approach versus standard protective ventilation in abdominal surgery
Ferrando. Lancet Respir Med. 2018; 6(3):193-203. doi: 10.1016/S2212-2600(18)30024-9.
Clinical Question
- In adult patients undergoing abdominal surgery, with intermediate-to-high-risk of post-operative pulmonary complications, will an individualised perioperative open-lung ventilation strategy (iPROVE), compared with standard protective ventilation, result in fewer post-operative complications during the first 7 days post surgery?
Background
- Low tidal volume ventilation has been demonstrated to prevent harm in critically ill patients with ARDS: ARMA trial
- This has been extrapolated and tested in peri-operative settings, with mixed outcomes
- The open-lung approach (OLA) takes a slightly different strategy, involving individualised, and often higher than traditionally applied, levels of Positive End Expiratory Pressure (PEEP)
- The recent ART trial in critically ill patients have suggested the recruitment and PEEP titration manoeuvres involved in the OLA may be harmful
- This trial attempts to investigate if OLA can reduce post-operative complications in patients undergoing abdominal surgery
Design
- A prospective, multi-centre, four-arm randomised controlled trial
- Ethics in accordance with the Declaration of Helsinki, the Convention of the European Council, and Spanish legislation for biomedical research
- Participants were enrolled by the investigators and randomly assigned, with a ratio of 1:1:1:1, into one of four lung-protective mechanical ventilation strategy groups
- Randomisation was thorough
- Used the Mersenne-Twister algorithm, a commonly used computer “pseudorandom number generator”, which passes most statistical tests of “randomness”
- Partial blinding was achieved
- Intraoperative data and data collected in the post-anaesthetic care unit (PACU) were collected by an unmasked investigator
- Post-operative data (i.e. on the ward) was collected by an investigator who was masked to treatment group
- Patients were masked to treatment group
- Power calculations based on an assumed risk of 25% for developing post-operative complication, and an absolute risk reduction of 12.5% in individualised treatment groups
- Powered at 80%
- Significance set at 0.05
- 920 patients required, 230 in each of the four arms
- 1012 recruited to account for dropout rate
- Interim analysis revealed a higher than expected complication rate, which could lead to a loss of power
- Post-hoc, patients were stratified by number of complications, categorised with an ordinal scale (0, 1-2, >2)
- To adjust for multiple comparisons, a p value of 0.016 was defined as the threshold for statistical significance in the primary outcome
- No adjustment was defined for secondary outcomes as these were not hypothesis testing end points
- Additional post-hoc analysis was hospital length of stay, upon which the effect of aggregated complications over the first 7 days, was analysed using Spearman’s correlation coefficient
Setting
- 21 teaching hospitals in Spain
- January 2015 – May 2016
Population
- Inclusion:
- Patients aged 18 years and older
- Scheduled for major abdominal surgery (laparoscopic or laparotomy) with expected duration >2 hours
- BMI < 35 kg/m2
- Intermediate-to-high-risk of post-operative pulmonary complications using the ARISCAT score
- Exclusion:
- Pregnant or breastfeeding
- Moderate-severe respiratory distress syndrome
- Cardiac Failure
- Diagnosis or suspicion of intracranial hypertension
- Mechanical ventilation during the previous 15 days (including CPAP)
- Presence of pneumothorax, giant bullae, COPD requiring oxygen therapy or CPAP
- Participation in another interventional trial
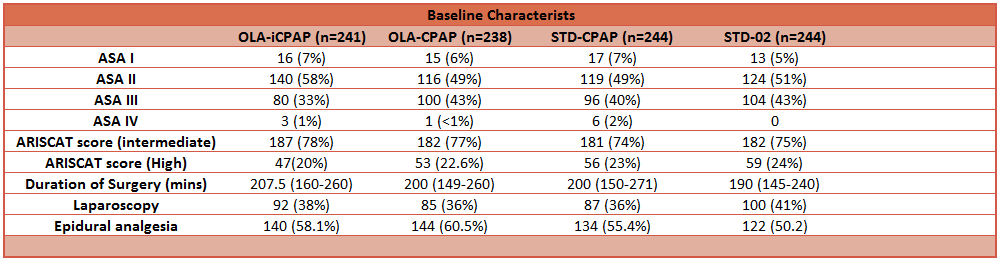
- 1012 patients randomly assigned
- 10 withdrew informed consent, 12 met exclusion criteria, further 23 excluded following screening failure
- 967 patients included in final analysis
- 241 in open-lung approach – post-op individualised CPAP group
- 238 in open-lung approach – post-op CPAP group
- 250 in standard intraoperative ventilation – post-op CPAP group
- 249 in standard intraoperative ventilation – standard post-operative oxygen therapy group
- Baseline characteristics and peri-operative parameters were similar between groups
Intervention
- All Patients were intubated
- 3 intervention groups against 1 control
- Allocation to one of four lung-protective perioperative ventilation strategies
- Open-lung approach – Post-op individualised CPAP (OLA-iCPAP)
- Individualised intraoperative ventilation
- Step-wise recruitment manoeuvre until airway pressure reached 40 cmH2O
- Followed by stepwise reduction in PEEP until optimal dynamic lung compliance (Cdyn) was reached
- Individualised PEEP set at 2 cmH2O above PEEP at which optimal Cdyn was reached
- Additional recruitment manoeuvres and PEEP titration performed if Cdyn decreased by >10% and SpO2 <96% after 5 mins of FiO2 0.21, assessed every 40 mins
- Post-operative CPAP of 5 cmH2O, or 10 cmH2O if BMI >30 kg/m2, was applied for 3 hours if SpO2 <96% while breathing room air in a supine position
- Open-lung approach – Post-op CPAP (OLA-CPAP)
- Individualised intraoperative ventilation (as above)
- Post-operative CPAP of 5 cmH2O, or 10 cmH2O if BMI >30 kg/m2, was applied for 3 hours regardless of SpO2
- Standard intraoperative ventilation – Post-op CPAP (STD-CPAP)
- Intraoperative lung-protective ventilation with 5 cmH2O fixed PEEP
- No recruitment manoeuvres
- Post-operative CPAP of 5 cmH2O, or 10 cmH2O if BMI >30 kg/m2, was applied for 3 hours regardless of SpO2
- Control: Standard intraoperative ventilation – Post-op O2 (STD-O2)
- Intraoperative lung-protective ventilation with 5 cmH2O fixed PEEP
- No recruitment manoeuvres
- Post-operatively patients received FiO2 0.5 via Venturi facemask
Control
- The control group was “standard intraoperative ventilation – Post-op O2” (STD-O2)
Management common to both groups
- Pre-oxygenation was done for 5 mins at FiO2 0.8 with a tight fitting facemask prior to induction of anaesthesia
- In all groups, intraoperative lung-protection mechanical ventilation settings included: volume control mode, 8 ml/kg predicted body-weight and maximum airway plateau pressure of 25 cmH2O
- FiO2 0.8 at extubation
- General post-operative management in the PACU followed established local protocols as determined by local physicians
Outcome
- Primary outcome: Composite of post-operative complications during the first 7 days post-operatively, including respiratory complications and systemic complications
- No significant differences in the primary outcomes in the modified intention-to-treat analysis
- Post-operative complications observed:
- OLA-iCPAP group: 46%
- OLA-CPAP group: 47%
- STD-CPAP group: 48%
- STD-O2 group: 51%
- Relative Risk (RR) compared to control (STD-O2):
- OLA-iCPAP group: RR 0.89 (95% CI 0.74–1.07; p=0.25)
- OLA-CPAP group: RR 0.91 (95% CI 0.76–1.09; p=0.35)
- STD-CPAP group: RR 0.95 (95% CI 0.80–1.14; p=0.65)
- Secondary outcome: Composite of pulmonary or systemic complications during the first 7 post-operative days and total complications between the 7th and 30th post-operative days; non-planned ICU admission; hospital re-admissions; length of stay in ICU and in hospital; death; and inflammatory markers
- OLA-iCPAP group had a lower incidence of post-operative pulmonary complications than the STD-O2 group
- RR 0.80; 95% CI 0.65-0.99; p=0.047
- OLA-iCPAP group had lower incidence of systemic complications (p=0.066)
- OLA-iCPAP group had a lower incidence of post-operative pulmonary complications than the STD-O2 group
- Tertiary and post-hoc analyses:
- Post-hoc composite of infectious complications; surgical site infection, sepsis, septic shock, and pneumonia
- OLA-iCPAP group had a lower incidence of infectious complications (p=0.014)
- Post-hoc composite of infectious complications; surgical site infection, sepsis, septic shock, and pneumonia
Authors’ Conclusions
- The different open-lung ventilation strategies compared in this trial did not reduce post-operative complications during the first 7 post-operative days
Strengths
- Multi-Centre, randomised control trial
- Good internal validity (accuracy of results)
- Independent randomisation using Mersenne-Twister algorithm; a widely used and recognised algorithm.
- This means that any investigators decision to recruit a patient could not be biased by any knowledge of which study group that patient would go into (allocation bias)
- Homogeneity of patient characteristics between groups
- There are no significant differences in key baseline variables
- Homogeneity of procedures and care
- Induction, maintenance, extubation and rescue manoeuvres for all groups were standardised and clinical care was based on “Enhanced Recovery after Surgery Programme”
- This reduces imbalance of treatment between groups that may have occurred from lack of blinding of clinicians
- Haemodynamic stability, fluid administration, use of vasopressors, blood loss, urine output, type of anaesthesia, type of surgery and surgery duration data published, and did not differ significantly between groups
- Independent randomisation using Mersenne-Twister algorithm; a widely used and recognised algorithm.
- Reasonable external validity (generalisability)
- There was a broad range of surgical procedures, allowing the results to be generalisable to most major abdominal surgery, though not to other surgery types
- Safe and ethical trial conduct
- Funders of study had no role in study design, data collection, data analysis, interpretation, or writing of the report
- All participants were managed with an intraoperative protective lung ventilation strategy (8 ml/kg tidal volume and minimum of 5 cmH2O PEEP) including the control group
- This is within current recommended practice guidelines, and avoided putting patients at risk with practices that have been shown to cause harm in previous studies
- Previous trials have used high tidal volume ventilation (10-12 ml/kg) and zero PEEP as the control group
Weaknesses
- Overly complex trial
- The study design, with four different groups, makes the paper difficult to read and it is hard to interpret the clinical relevance
- Inclusion criteria of “intermediate-high-risk of pulmonary complication”, was automatically met by the inclusion criteria of “abdominal surgery” and “duration >2hours” using the ARISCAT scoring system, rendering the use of this scoring system redundant
- Poor biological plausibility
- The overall difference in ventilation strategies between groups was relatively minor, with the duration of post-operative CPAP interventions only lasting for three hours post-surgery, before the patients rejoined routine post-operative care
- This three-hour CPAP intervention is fairly minimal, given the primary outcome was based on complications seen over seven post-operative days, perhaps making it unsurprising that there was no significant differences in the primary outcome
- Composite outcomes
- Primary outcome was based on a composite of multiple pulmonary and systemic complications, making clinical relevance difficult to assess as all individual events of equal weighting despite some being clinically less important
- Some internal validity concerns
- Control group had significantly higher incidence of hypoxaemia requiring rescue manoeuvres with increased PEEP
- Application of rescue manoeuvres in control group may have led to a bias resulting in a reduced difference observed between groups, although it would have been unethical to not rescue hypoxic episodes
- Unable to mask group allocation from anaesthetist and PACU staff
- Risk of bias from differential application of care protocols
- Different rates of epidural analgesia between groups (control group: 50.2% vs intervention groups: 55.4%, 58.1% and 60.5%)
- Pulmonary complications may be sensitive to application of epidural analgesia
- This small difference in epidural incidence rate may have biased in favour of identifying a difference between the control group and intervention groups
- Control group had significantly higher incidence of hypoxaemia requiring rescue manoeuvres with increased PEEP
- Poor generalisability to other important patient populations
- Higher risk patients, such as BMI>35 kg/m2, were excluded
- It would arguably be more useful to know the impact of the iPROVE strategy in higher risk populations, such as those with obesity or known lung disease
- Statistical power was lower than planned
- Higher than expected overall complication rate led to loss of statistical power, and a removal of comparison between all groups. (that is, comparisons only made with control
The Bottom Line
- Intraoperative individualised ventilation aimed at minimising lung de-recruitment, combined with prophylactic post-operative CPAP in patients with clinical signs of de-recruitment (SpO2 <96% on room air), did not show a statistically significant reduction in the incidence of post-operative pulmonary complications in this study.
- Further appropriately powered studies are required to clarify the non-statistically significant benefits shown, and demonstrate “optimum ventilation strategy” in the peri-operative period.
- I will continue my current practice of seeking to avoid de-recruitment, with adequate use of PEEP and recruitment manoeuvres, while avoiding excessive ventilator pressures.
External Links
- [article] Individualised perioperative open-ling approach versus standard protective ventilation in abdominal surgery (iPROVE): a randomised controlled trial.
- [further reading] A Trial of Intraoperative Low-Tidal-Volume Ventilation in Abdominal Surgery
Metadata
Summary author: Doug Tunney
Summary date: 15 February 2019
Peer-review editor: Duncan Chambler



