IDEAL-ICU
Timing of Renal-Replacement Therapy in Patients with Acute Kidney Injury and Sepsis
Barba. NEJM 2018;379:1431-1442
Clinical Question
- In patients with septic shock and severe acute kidney injury, does early vs. delayed renal replacement therapy improve 90 day mortality?
Background
- Acute kidney injury is a common occurrence in patients with septic shock. The decision as to when to start renal replacement therapy is controversial
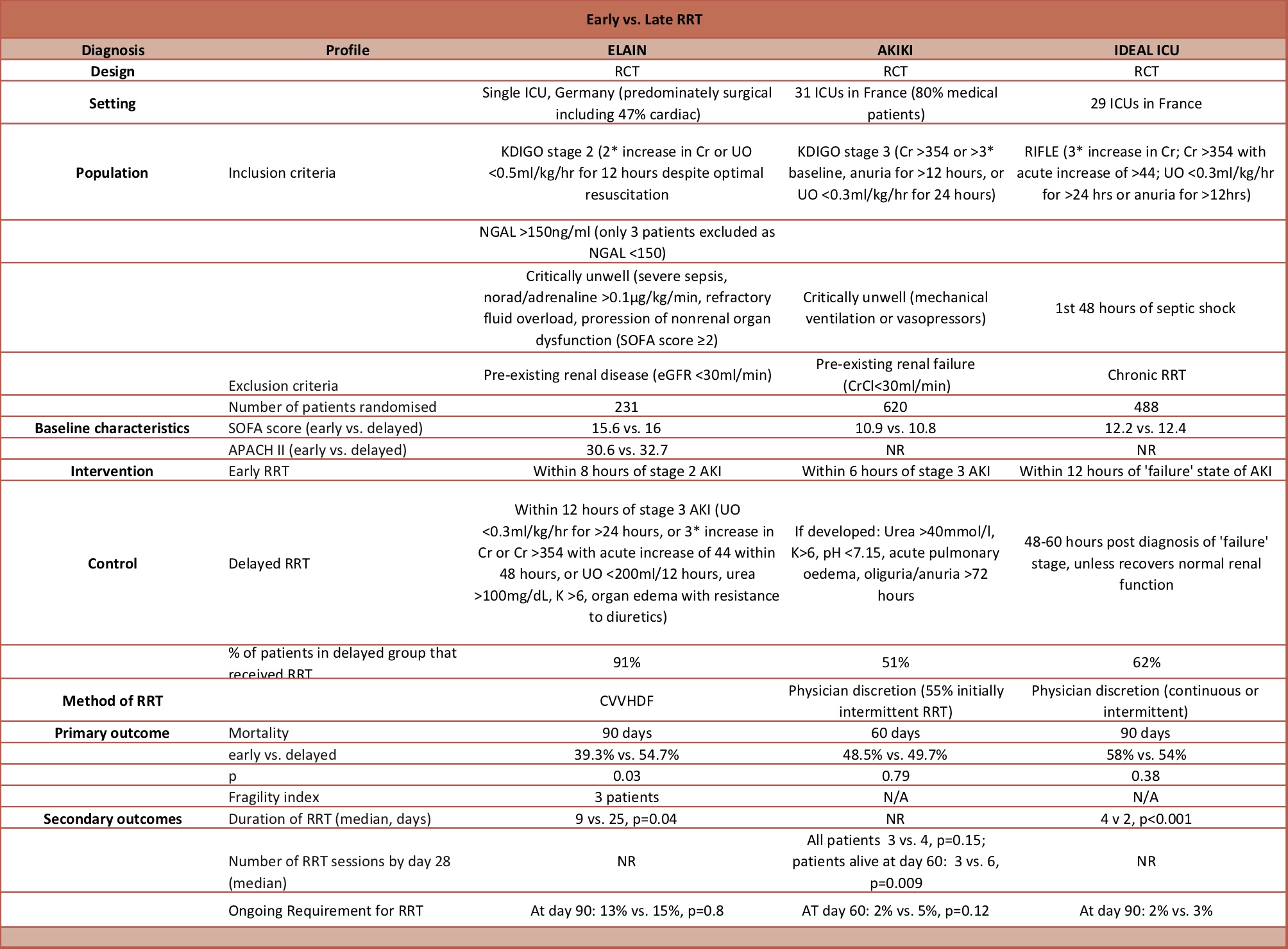
- The AKIKI trial reported no difference in mortality with an early vs. a delayed approach, whereas the ELAIN trial found a significant mortality benefit with the early approach
- There are some key differences between these two randomized trials that are summarized in our previous editorial
Design
- Randomised controlled trial
- Open-label / non-blinded
- Computer generated randomisation, stratification according to age, centre and SOFA score
- Intention to treat analysis
- Registered on clinicaltrials.gov
- 864 patients required to give 80% power, to detect a 10% absolute risk reduction from a baseline mortality of 55%, with a 2 sided alpha level of 0.05
- 2 planned interim analyses
- Stopped early due to futility
- Conditional power calculated when trial terminated was 51%
Setting
- 29 ICUs in France (22 university teaching hospital and 7 general hospitals)
- Data collected July 2012 – October 2016
Population
- Inclusion: Adult patients with septic shock and acute renal failure
- Septic shock defined as severe sepsis with >=2 SIRS criteria and need for vasopressors despite adequate vascular filling
- Within 48 hours of starting vasopressors
- Acute renal failure defined as “failure” stage of RIFLE classification i.e. the presence of >=1 of the following:
- Increased creatinine
- x3 baseline value, or
- >4 mg/dl (350 umol/l) accompanied by rapid increase of >0.5 mg/dl (44 umol/l)
- Oliguria <0.3ml/kg/hr for 12 hours
- Anuria: diuresis <100ml for 12 hours
- Increased creatinine
- Exclusion: Chronic renal failure requiring dialysis, obstructive renal failure, emergency criteria for immediate haemodialysis (K > 6.5, pH <7.15 or pulmonary oedema by fluid overload), moribund or unlikely to survive to 28 days because of uncontrolled co-morbitiies, DNAR in place
- 488 patients randomised out of 1728 who were assessed for eligibility
- Comparing intervention vs. control group – no significant differences in baseline characteristics
- Age: 69 vs. 69
- Male: 58% vs. 64%
- Chronic renal failure: 13% vs. 18%
- Diabetes: 33% vs. 29%
- SOFA score at enrollement: 12.2 vs. 12.4
- Exposure to at least 1 nephrotoxic drug in preceding 4 days: 52% vs. 44%
- Invasive mechanical ventilation: 89% vs. 88%
- Vasopressor requirement: 100% vs. 100%
- Diagnostic criteria for ‘failure’ stage of RIFLE classification
- Oliguria: 35% vs. 33%
- Anuria: 34% vs. 36%
- Serum creatinine 3 times baseline: 63% vs. 62%
- Fluid balance pre-enrollement ml/24 hour: +3194 vs. +3211
Intervention
- Early initiation of RRT
- Start of RRT within 12 hours of documentation of ‘failure-stage’ acute kidney injury
- 97% of patients received RRT
Control
- Deferred initiation of RRT
- RRT initiated after a delay of 48 hours post-diagnosis of ‘failure-stage’ of acute kidney injury, if renal function had not spontaneously recovered or criteria for emergency RRT had been met
- 62% of patients received RRT at any time
- 17% of patients received RRT earlier than 48 hours due to criteria for emergent RRT being met
- 29% did not receive RRT because renal function spontaneosly recovered
- 8% died before RRT initiated
Management common to both groups
- Choice of RRT (intermittent vs. continuous) was at discretion of clinician, but had to adhere to protocol instructions for setting
• In cases of life threatening conditions (K >6.5mmol, metabolic acidosis with pH < 7.15, pulmonary oedema that was refractory to diuretics) within the 48 hours after randomisation, RRT initiated as soon as possible
• In case of improvement of renal function within the 48 hours post randomisation (return of spontaneous urine output >1000ml/24hr or >2000ml/hr with diuretics), RRT is not mandatory
Outcome
- Primary outcome: All cause 90 day mortality – no significant difference
- 58% in early strategy vs. 54% in delayed, p=0.38
- Secondary outcomes – comparing early vs. delayed strategy
- Significantly lower:
- Median time from diagnosis of AKI to RRT
- 7.6 vs. 51.5 hours, p<0.001
- Days free of RRT
- 12 vs. 16, p=0.0006
- Episodes of hyperkalaemia
- 0% vs. 4%, p=0.03
- Median time from diagnosis of AKI to RRT
- No significant differences in:
- Median days free of mechanical ventilation: 2 vs. 3
- Median days free of vasopressors: 16 vs. 17
- Median length of hospital stay: 23 vs. 23 days
- Dependence on RRT amongst survivors at day 90: 2% vs. 3%
- Fluid overload: <1% vs. 4%
- Severe bleeding event: 5% vs. 6%
- Significantly lower:
Authors’ Conclusions
- In patients with septic shock and severe acute kidney injury there was no difference in mortality for patients assigned to an early compared with a late strategy for renal replacement therapy
Strengths
- Randomised controlled trial
- Patient centered outcome
- Intention to treat analysis
- Registered on clinicaltrials.gov
- Minimal loss to follow up
Weaknesses
- Non-blinded – unrealistic to blind clinicians but authors could have been blinded during data collection and analysis
- Stopped early due to futility with resultant decrease in power
- Use of both continuous and intermittent RRT allowed which is not consistent with practice in UK
The Bottom Line
- In patients with septic shock and acute kidney injury, this randomized controlled trial that was stopped early due to futility, found no difference in mortality with the use of early vs. delayed renal replacement therapy
- Use of the delayed strategy resulted in a reduction of the number of patients that required renal replacement therapy
External Links
- [article] Timing of Renal-Replacement Therapy in Patients with Acute Kidney Injury and Sepsis
- [further reading] AKIKI trial
- [further reading] ELAIN trial
- [further reading] ELAIN Follow up
- [further reading] 2016 TBL editorial: early vs. late RRT
Metadata
Summary author: @davidslessor
Summary date: 07/11/18
Peer-review editor: @DuncanChambler



