Pupillometry Thresholds for Neuroprognostication

Validating quantitative pupillometry thresholds for neuroprognostication after out‑of‑hospital cardiac arrest. A predefined substudy of the Blood Pressure and Oxygenations Targets After Cardiac Arrest (BOX)‑trial
Nyholm. Intensive Care Med 2024; 50:1484–1495. doi.org/10.1007/s00134-024-07574-6
Clinical Question
- In adult out-of-hospital cardiac arrest (OHCA) survivors of presumed cardiac cause who are comatose post-admission, do automated pupillometry thresholds of quantitatively assessed pupillary light reflex (qPLR) < 4% and Neurological Pupil index (NPi) ≤ 2 predict unfavourable neurological outcome with zero-percent false-positive rate?
Background
- Many patients who achieve return of spontaneous circulation (ROSC) following cardiac arrest suffer hypoxic–ischemic brain injury
- Neuroprognostication is essential to identify those for whom treatment is futile and to inform decision making regarding withdrawal of life-sustaining treatment
- Assessment of pupillary reflexes is an important part of the neuroprognostication process but there is significant inter-observer variability when manually assessing pupillary reflexes and guidelines recommend automated pupillometers for neuroprognostication
- Several studies have confirmed the significant prognostic value of quantitatively assessed pupillary light reflex (qPLR) and Neurological Pupil index (NPi) measures via automated pupillometry, however results on absolute values differ across studies
Design
- Diagnostic accuracy study
- Prospective observational design
- Predefined substudy of the BOX RCT
- All patient received protocolised post-resuscitation care
- Withdrawal of life sustaining treatment made no earlier than 72 hours after ending sedation, based on specified criteria
- Blinding of outcome assessors to test of interest results
- Blinding of clinicians to automated pupillometry results
Setting
- 2 Danish tertiary cardiac arrest centers
- Enrolment from March 2017 until December 2021
Population
- Inclusion:
- > 18 years old
- OHCA survivors (presumed cardiac origin)
- Sustained ROSC >20 mins
- Comatose at admission (GCS <8)
- Exclusion:
- Pre-existing ophthalmic conditions affecting pupil movement
- Lack of pupillometry data
- Known pre-arrest CPC 3 or 4
- Females of childbearing potential (unless a negative HCG test ruled out pregnancy within the inclusion window)
- In-hospital cardiac arrest (IHCA)
- OHCA of presumed non-cardiac cause
- Suspected or confirmed acute intracranial bleeding
- Suspected or confirmed acute stroke
- Unwitnessed asystole
- Known limitations in therapy and Do Not Resuscitate-order
- Known disease making 180 days survival unlikely
- >4hours (240min)from ROSC to screening
- Systolic blood pressure < 80 mmHg despite fluid loading/vasopressor and/or inotropic medication intra-aortic balloon pump/axial flow device
- Temperature on admission < 30°C
- 789 assessed, 710 included
- 71 lacked pupillometry data
- 8 had a history of cataract surgery
- Baseline characteristics
- Mean age: 63
- Male: 82%
- Mean time-to-ROSC: 21 minutes
- Primary shockable rhythm: 91%
- Witnessed OOHCA: 85%
- Bystander CPR 89%
- Pupillometry conducted unless awakened or died
- 100% patients on admission
- 96% at 24 hours
- 76% at 48 hours
- 42% at 72 hours – after 72 h 5% patients had died, 26% were still unconscious with Glasgow Motor Score ≤ 3
Tests of Interest
- Automated pupillometry: 2 distinct measures obtained using NPi-200 pupillometer
- Quantitatively assessed pupillary light reflex (qPLR)
- Percentage of pupillary constriction to a calibrated light stimulus (1000 Lux)
- Threshold of qPLR < 4% tested
- Neurological Pupil index (NPi)
- Composite score integrating multiple pupillary variables (size, latency, constriction, and dilation velocity)
- Measured from 0 to 5: ≥ 3 is considered normal, < 3 indicates abnormal reactivity (0 indicates a non-reactive/absent response)
- Threshold of NPi ≤ 2 tested
- NPi is a proprietary measurement and requires a NeurOptics pupillometer for measurement. Full NPi algorithm including components and calculations remain unpublished
- Automated pupillometry conducted at admission, 24 hours, 48 hours and 72 hours using NPi-200 pupillometers unless awakened or died
- Lowest value of the two eyes defined threshold values
- Quantitatively assessed pupillary light reflex (qPLR)
- Neuron-specific enolase (NSE)
- Measured at 48 hours
- Threshold of > 60 μg/L tested
- Combined prediction of 48-h plasma NSE > 60 μg/L and pupillometry performed in patients with Glasgow Motor Score (M) ≤ 3 at ≥ 72 h. The combination of pupillometry and NSE thresholds was performed sequentially with a conditional subsequent retest (qPLR < 4 or NPi ≤ 2) if the first test was negative (NSE ≤ 60 μg/L). The overall test was positive if either test was positive
Gold Standard Investigation
- Neurological function defined by Cerebral Performance Category (CPC) score assessed at follow-up no earlier than 90 days. Assessment performed by trained personnel blinded to the pupillometry results, either in-person, by telephone interview or review of medical records
Outcome
- Primary outcome:
- Unfavourable neurological outcome (Cerebral Performance Category (CPC) score ≥ 3)
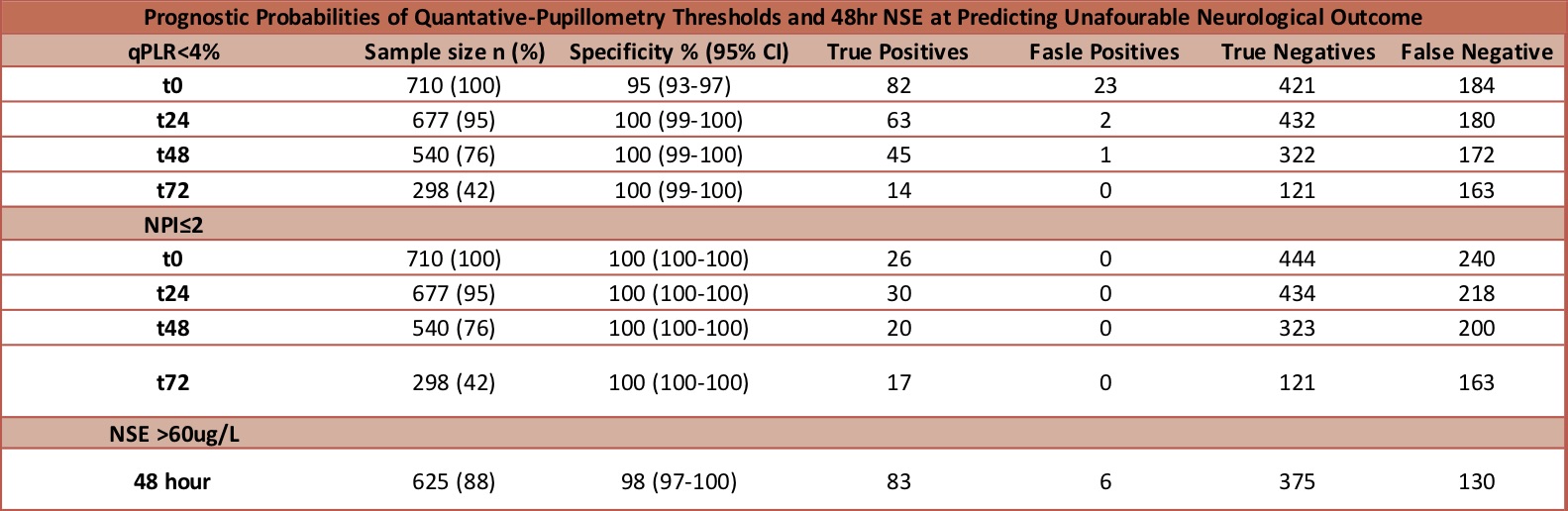
- qPLR < 4% measured from 24-hours until 72-hours predicted unfavourable neurological outcome with 0% false-positive rate (FPR). Positive predictive value (PPV) ranged from 97-100%
- NPi ≤ 2 measured from admission until 72-hours predicted unfavourable neurological outcome with 0% FPR. PPV was 100%
- Sensitivity highest when measured at 24-hours – 26% for qPLR < 4%, 12% for NPi ≤ 2
- Unfavourable neurological outcome (Cerebral Performance Category (CPC) score ≥ 3)
- Secondary outcomes:
- All-cause death within 365 days
- 93% in patients with qPLR < 4% measured at 48-hours, 33% if qPLR ≥4%
- 100% in patients with NPi ≤ 2 measured at 48-hours, 36% if NPi >2
- Median 48-hour plasma NSE
- NSE > 60µg/L predicted unfavourable neurological outcome with 2% FPR and sensitivity of 39%. 95% PPV
- In patients who remained comatose at ≥ 72 hours with Glasgow Motor Score ≤ 3, NSE predicted unfavourable neurological outcome with 0% FPR and sensitivity of 42%
- When combined with pupillometry measured at 48-hours sensitivity was improved – 55% (pQLR < 4%) and 50% (NSi ≤ 2)
- Alternative measures of neurological outcome
- pQLR < 4% and NPi ≤ 2 predicted unfavourable neurological outcome as defined by modified Rankin scale (mRS) ≥ 3 with similar results to CPC score ≥ 3
- MOCA scores only available for 1 patient with pQLR < 4% and unavailable for all patients with NSi ≤ 2
- All-cause death within 365 days
Authors’ Conclusions
- Quantitative pupillometry after OHCA, with specific thresholds of qPLR < 4% and the NPi ≤ 2, predicted unfavourable neurological outcomes with zero-percent FPR
Strengths
- Excellent specificity of pupillometry thresholds demonstrated including 0% FPR
- Combination with NSE measurement improved sensitivity without affecting FPR
- Patient-centred primary outcome
- Large population
- Clinical staff blinded to all automated pupillometry
- All patients followed-up and neurological status assessed
Weaknesses
- Observational study without randomisation or control
- Majority male population
- Study only performed in 2 centres in 1 country
- 71 patients (9%) excluded due to lack of pupillometry data
- Poor sensitivity for automated pupillometry, even when combined with NSE
- Pupillometry not performed on patients who have awakened – it is unclear how this may impact results
- No control for ambient light
- NPi is a proprietary measurement and requires a NeurOptics pupillometer for measurement. NPi algorithm including components and calculations unpublished
- MOCA unavailable for majority of patients
The Bottom Line
- This study demonstrates that for patients admitted to hospital with ROSC after an OOHCA of cardiac cause, pupillometry thresholds of qPLR < 4% and NPi ≤ 2 predict an unfavourable neurological outcome with 0% FPR
- Sensitivity was poor, even when combined with NSE
- Neuroprognostication after OOHCA is challenging and the automated pupillometry thresholds demonstrated by the authors provide objective evidence to aid in this process
External Links
Metadata
Summary author: Stephen Waite – @etomid8
Summary date: 03/11/2024
Peer-review editor: David Slessor
Photo by Ion Fet on Unsplash



