DECRA
Decompressive Craniectomy in Diffuse Traumatic Brain Injury
Cooper D.J. NEJM, 2011; DOI: 10.1056/NEJMoa1102077
Clinical Question
- In patients admitted to ICU with severe diffuse traumatic brain injury (TBI) and refractory raised intracranial pressure (ICP), does early decompressive craniectomy improve functional outcomes when compared with continued medical management?
Background
- Traumatic brain injury is a common reason for ICU admission and is associated with high morbidity and mortality.
- Raised intracranial pressure is an important cause of secondary brain injury and many patients with TBI have refractory raised ICP which does not respond to first tier medical interventions
- Decompressive craniectomy is used as a treatment for refractory raised ICP in TBI, with some retrospective trials suggesting a mortality benefit
- However, no large randomised-controlled trials had previously been conducted
Design
- International, multi-centre, randomised controlled trial
- Randomisation within 72 hours of injury
- Trigger for randomisation: refractory raised ICP – defined as ICP >20mmHg for 15 mins (continuous or intermittent) within 1 hour despite tier 1 interventions
- Stratified according to centre and ICP monitoring technique
- Randomised in blocks of two or four patients
- Treating teams were non-blinded to allocation however outcomes were evaluated by three blinded assessors
- Structured telephone assessment used
- Intention-to-treat analysis
- Originally designed to detect an increase in the proportion of favourable outcomes (defined as GOS-E of 5-8) from 30% to 50% (power of 80%) with a sample size of 210 patients.
- Following interim analysis (Jan 2007) the primary outcome was revised to be median GOS-E with a sample size of 150 required to detect a difference of 1.5 between groups via ordinal logistic regression. This was done to allow the study to be completed in a shorter timeframe
- Written informed consent from NOK
Setting
- 15 ICUs in Australia, New Zealand, and Saudi Arabia
- All with advanced neurosurgical management capabilities
- Dec 2002 – April 2010
Population
- Inclusion Criteria:
- Severe, non-penetrating TBI
- Defined as either GCS 3-8 (post-resuscitation or pre-intubation), or
- Marshall Class III injury on CT imaging
- < 72 hours from injury
- Severe, non-penetrating TBI
- Exclusion Criteria:
- Not deemed suitable for full active treatment
- Dilated, unreactive pupils
- Mass lesions (unless too small to require surgery)
- Spinal cord injury
- Arrest at scene
- ICP controlled
- 3478 patients with TBI assessed for eligibility:
- 3302 excluded
- Majority due to exclusion criteria
- 344 other
- 21 additionally declined consent
- 155 randomised
- 73 allocated to craniectomy
- 82 allocated to standard care
- 3302 excluded
- Baseline characteristics
- Very similar between the two groups, except for pupil reactivity (comparing craniectomy vs standard care group):
- Median age: 23.7 vs 24.6
- Male: 81% vs 74%
- Clinical parameters prior to randomisation
- Median SBP 135.4 vs 135.7
- Hypotension 33% vs 30%
- Hypoxaemia 25% vs 29%
- Neurological status
- Median GCS: 5 vs 6
- Median motor score: 3 vs 3
- Bilateral unreactive pupils: 27% vs 12%
- Injury severity
- Median Injury Severity Score: 33 vs 32
- Marshall class II: 23% vs 33%
- Marshall class III or IV: 73% vs 65%
- Marshall class VI: 4% vs 2%
- Mechanism of injury
- MVA/MBA: 64% vs 68%
- Bicycle accident: 6% vs 2%
- Pedestrian accident: 7% vs 5%
- Other: 23% vs 25%
- Median time from injury to hospital: 1 hour vs 1.2 hours
- Median time from injury to randomisation: 35.2 hours vs 34.8 hours
Intervention
- Decompressive craniectomy plus standard care
- Standardised surgical approach:
- Large bifrontotemporoparietal craniectomy with bilateral dural opening. The sagittal sinus and falx cerebri were not divided.
Control
- Standard care based on BTF guidelines
- Protocol allowed lifesaving decompressive craniectomy after 72 hours from admission
Management common to both groups
- All patients had ICP monitoring (either EVD or parenchymal catheter)
- Treatment whenever ICP >20mmHg
- First tier interventions included:
- Sedation optimisation
- PaCO2 normalisation
- Mannitol
- Hypertonic saline
- Neuromuscular blockade
- External ventricular drainage
- Second tier interventions for refractory raised ICP included:
- Mild hypothermia (35°C)
- Barbiturates
- Second tier interventions could be used following randomisation in the surgical group
Outcome
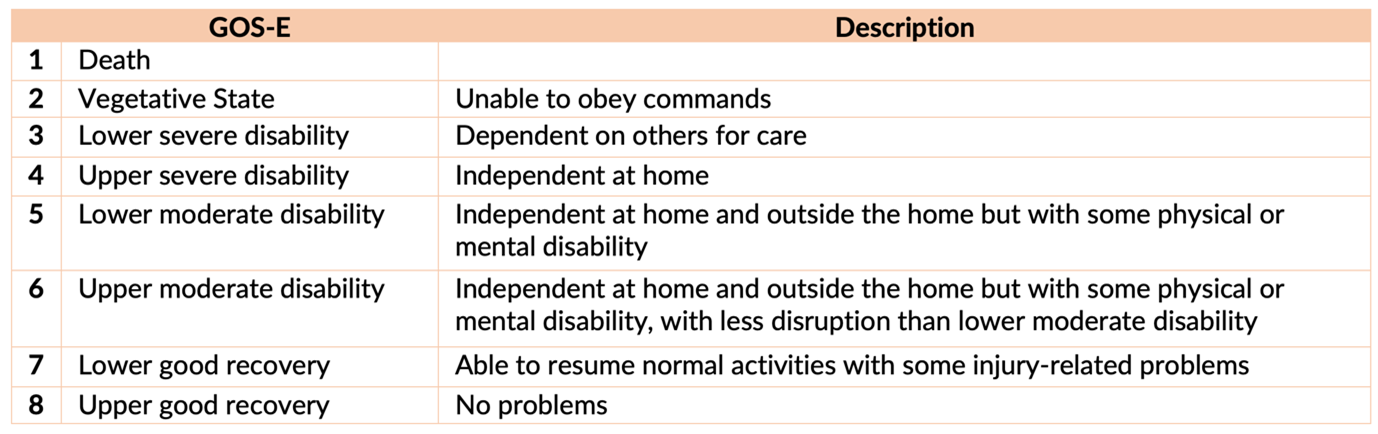
- Primary outcome:
- Median Extended Glasgow Outcome Scale (GOS-E) at 6 months
- 3 (craniectomy) vs 4 (standard care)
- OR 1.84 (95% CI 1.05-3.24), p=0.03
- 3 (craniectomy) vs 4 (standard care)
- Median Extended Glasgow Outcome Scale (GOS-E) at 6 months
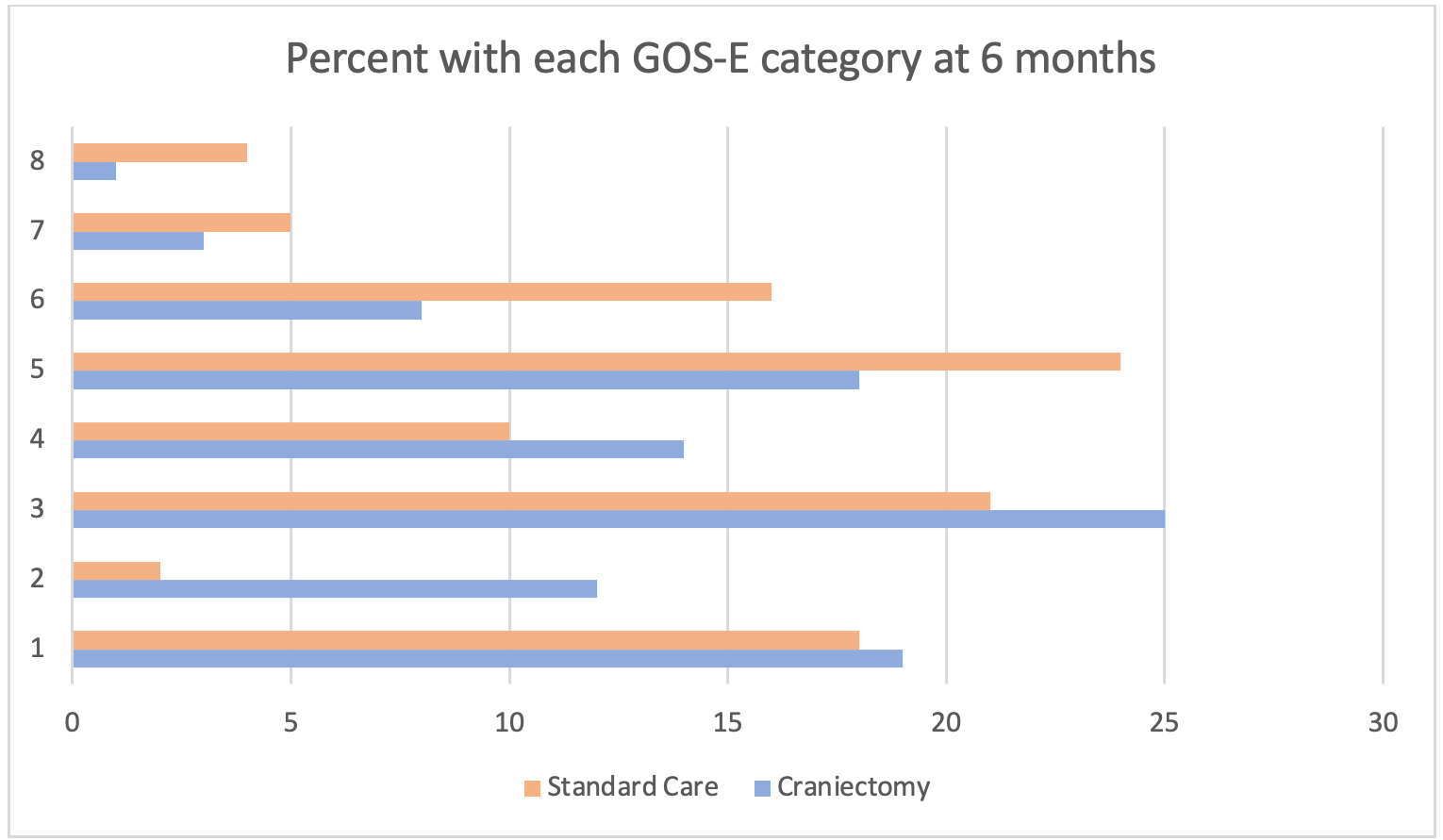
- Secondary outcomes:
- Proportion of unfavourable outcomes (GOS-E 1-4) at 6 months
- 70% (craniectomy) vs 51% (standard care),
- OR 2.21 (95% CI 1.14 – 4.26), p=0.02
- 70% (craniectomy) vs 51% (standard care),
- Mortality
- 19% vs 18%
- Intracranial pressure
- Mean ICP after randomisation: 14.4mmHg vs 19.1mmHg, p<0.001
- Hours with ICP >20mmHg: 9.2 vs 30.0, p<0.001
- As a result, the surgical group required significantly less first and second tier medical interventions post randomisation
- Duration of hospital intervention
- Days of mechanical ventilation: 11 vs 15, p<0.001
- Days in ICU: 13 vs 18, p<0.001
- Days in hospital 28 vs 37, p=0.82
- Proportion of unfavourable outcomes (GOS-E 1-4) at 6 months
- Subgroup Analyses
- Adjusted comparisons for age, baseline GCS, motor score and Marshall score did not demonstrate any significant difference in results for GOS-E and unfavourable outcome
- Post hoc adjustment for pupil reactivity meant the difference in functional outcomes were no longer statistically significant:
- GOS-E score: adjusted OR 1.53 (95% CI 0.86 – 2.73), p=0.15
- Unfavourable outcome: adjusted OR 1.90 (95% CI 0.95 – 3.79), p=0.07
Authors’ Conclusions
- In adults with severe diffuse traumatic brain injury and refractory intracranial hypertension, early bifrontotemporoparietal decompressive craniectomy decreased intracranial pressure and the length of stay in the ICU but was associated with more unfavourable outcomes at 6 months
Strengths
- Large, randomised controlled trial across 15 ICUs in 3 countries
- No patients lost to follow-up or withdrawn consent
- 96% of patients received assigned treatment following randomisation
- 3 patients (4%) of intervention group did not receive craniectomy, 2 due to stabilisation of ICPs and 1 due to incorrect randomisation
- Standardised protocol for medical management which was consistent across sites and was based on Brain Trauma Foundation guidelines
- GOS-E is a well validated tool for assessing functional status following brain injury
Weaknesses
- Treatment teams unable to be blinded to group assignment due to nature of neurosurgical procedure
- Over a third of patients were recruited from one centre (and 88% of patients were from Australia or New Zealand)
- Long recruitment period of 8 years
- Some clinicians suggest the cut-off of ICP >20mmHg for 15 mins is too low/early to trigger surgical intervention
- Hypothermia to 35°C (which is now thought to be potentially harmful) was able to be used as a second-tier intervention, however its use was not reported
- Primary outcome changed midway through trial
- However both outcomes were reported and both statistically significant at the end of the trial
- Difference in pupil reactivity at baseline is a potential confounding factor and adjusted outcomes were no longer statistically significant
- There was crossover from the standard group to the craniectomy group:
- Crossover was allowed >72 hours is still considered salvageable and had an uncontrollable ICP despite thiopentone infusion
- Nearly 1/4 of patients crossed over:
- 5% of control group received craniectomy prior to 72 hours
- 18% of the standard care group underwent decompressive craniectomy after 72 hours as a life-saving procedure
- This may be why there is no mortality difference between groups
- 56 out of 70 craniectomy patients underwent cranioplasty within 6 months which may have had additional complications contributing to 6 month functional outcomes
- Overall complications between the two groups were similar
- This trial specifically assessed bifrontotemporoparietal without division of the falx cerebri. Other surgical techniques may have more favourable outcomes and/or less complications
- Patients with mass lesions were excluded from the trial and therefore the results cannot be generalised to this population
The Bottom Line
- In patients with diffuse TBI, early bifrontotemporoparietal decompressive craniectomy effectively reduced ICP but did not improve functional outcomes.
- While I will continue to seek neurosurgical intervention for patients with mass lesions, the decision to proceed to decompressive craniectomy in patients with diffuse TBI is less clear and with the increased chance of poor functional outcomes, patient values and other individual circumstances need to be considered
What research has been published since this trial?
- Within this trial patients were randomised to receive early decompressive craniectomy
- Subsequently, the RESCUEicp which was published in 2016 performed decompressive craniectomy as a last tier intervention
- There have been no other multi-centre randomised control trials looking at decompressive craniectomy in diffuse TBI
- In patients with traumatic intracerebral haemorrhage the STITCH trauma was published in 2015
External Links
- [article] Decompressive Craniectomy in Diffuse Traumatic Brain Injury
- [Editorial] Clinical Value of Decompressive Craniectomy
Metadata
Summary author: Eliza Mason
Summary date: 1st April 2022
Peer-review editor: George Walker / Alastair Brown
Picture by: Unsplash / Buddhi Kumar Shrestha



